
Prescribing PrEP with Confidence: Quick Videos to Get Started
Getting Practical with PrEP: Patient Candidacy, Medication Choices, and Side Effects
Short videos. Trusted facts.
With Dr. Jonathan Shuter, Dr. Uriel Felsen, Dr. Raffaele M. Bernardo, and Dr. Rasika Karnik
- Who is PrEP For?
- Options for PrEP
- Side Effects of PrEP
- View the entire webinar here
Who is PrEP For?
Transcript:
Dr. Uriel R. Felsen:
PrEP is for anyone that isn’t already living with HIV, and is at risk for acquiring HIV. So there are some ways to think about, some populations who may be more at risk for HIV. But I think the most important take home point for everyone to come home, you know, everyone who’s watching this to understand, is that it’s really for anyone that doesn’t already have HIV, and that is interested in protecting themselves from acquiring HIV, either through sex or through intravenous drug use.
Options for PrEP
Transcript:
Dr. Raffaele Bernardo:
So there are currently three medications that are FDA-approved for HIV pre-exposure prophylaxis.
Two of these medications come in the form of an oral tablet that’s taken once daily, and the third is actually the first long acting injectable for HIV pre-exposure prophylaxis. But all three are FDA-approved, and all three, as long as they’re taken as prescribed, are highly effective at preventing HIV infection. The two tablets are single fixed-dose combination tablets of two different medications of the brand names. One is Truvada, the other is Descovy, and the long acting injectable goes by the brand name Apretude. Apretude is given one month back to back for the first two months, and then every other month thereafter.
Dr. Uriel R. Felsen:
It’s important to remember that there are three choices, but not all choices are necessarily for all different folks. There’s an option, anybody that’s interested in PrEP, there is an option. Dr. Bernardo mentioned Descovy and Truvada. Both of them contain tenofovir and emtricitabine, but they contain different formulations of the tenofovir.
And currently, it’s really Truvada that is approved for cis men, cis women, and transgender men and transgender women, whereas Descovy is actually not approved for HIV prevention for anyone that’s at risk for acquiring HIV through vaginal sex. So that would be for cis women or potentially trans men.
Side Effects of PrEP
Transcript:
Dr. Jonathan Shuter:
These medications are extremely well tolerated. So almost anyone who puts any new pill in their mouth and swallows it could get some nausea. So there is, you know, a certain incidence of nausea and GI upset, associated with the two oral preparations. There were larger earlier concerns with the potential for renal effects and for bone effects with the tenofovir-containing preparations which are both of the oral medications. But most of those fears and concerns have been allayed by the collective experience that that significant renal toxicity or bone toxicity are rare.
And so those are really the common side effects with the pills. With the injection, it is basically what you would expect. With the injection, they get injection in site pain, and it is rare that that is severe enough that it causes discontinuation of the medicine, and that tends to get less with subsequent injections.
Dr. Raffaele Bernardo:
I’ll add, with the nausea that’s occasionally seen, almost always is self limiting, and within a week or so of daily use, the nausea actually goes away without any particular intervention. So I will often counsel my patients and say, while it’s rare, you may experience some nausea in the first few days. If it’s not too uncomfortable, keep taking your pill daily, and almost invariably the nausea self resolves within a couple of days when it happens. But to Dr. Shuter’s point, these side effects are typically very rare.
Recorded on September 30th, 2024 at 8 pm ET

PrEP in Practice: Key Steps. Quick videos
Clinical Foundations for PrEP: Conversations, Coverage, and Continuity of Care
Short videos. Trusted facts.
With Dr. Jonathan Shuter, Dr. Uriel Felsen, Dr. Raffaele M. Bernardo, and Dr. Rasika Karnik
- Taking a Sexual History
- Insurance Coverage for PrEP
- Starting PrEP
- Tips for PrEP Adherence
- Stopping PrEP
- View the entire webinar here
Taking a Sexual History
Transcript:
Dr. Raffaele Bernardo:
These are important conversations we should be having with all of our patients, regardless of age, sex, race gender, because once you standardize it, it becomes easier, I think, more natural when you’re having these conversations, and how you start off having these conversations is largely a personal preference.
I usually will start off by saying something like. The next thing I would like to talk about is your sexual health. I feel like this is a topic that often goes unaddressed, and is just as important as every other part of your health. So if you don’t mind, I’d like to ask you some questions.
And then from there I try to start off with open, ended questions. I try to let the patients lead the conversation themselves, because number one, sometimes it’s more natural that way, and sometimes patients are more comfortable sort of just ad lib. Talking about their sexual history, but if you find that they are stuttering, or they have a hard time giving you the information you need, you can start asking some more pointed questions, and this could be something as simple as can you tell me a little bit about who you’re having sex with? What are the genders of the people that you’re having sex? With? What body parts are you using to have sex? What methods are you using to prevent pregnancy? What methods are you using to prevent HIV infection?
There are lots of these different things online that you can look for to help organize your sexual history-taking to make it easier. But I think the important thing is that you try to create consistency with having these conversations because they’ll eventually happen more naturally. But it’s important to be comprehensive, because the question you don’t ask leads to the answer you don’t get, and it’s a missed opportunity to perhaps talk about some sort of preventative strategy with your patient.
The other thing that I will add as well. The questions you ask are part of it. But I think the environment you create is just as if not more important than the questions you’re asking. Because anyone in this audience can think about perhaps being asked these questions in two very different scenarios, right? A very sort of whitewashed office, very sort of sterile environment versus an environment that perhaps has some signage on the wall sort of promoting sexual health, you know, depending on the population you’re serving. For example, I’m the medical director for a comprehensive LGBTQ-plus practice in New Jersey. So in our office, although we serve all types of individuals, we do have very subtle gestures of support toward the community. So we have, for example, a pride flag in the waiting room. We have nice modern pieces of art that tie-in the LGBTQ-plus colors as well. So these subtle hints of support, I think, are also very important. You want to create an environment that welcomes these conversations. So I think again, the environment you’re creating is just as important, if not more important, than the actual questions that you’re asking your patients.
Insurance Coverage for PrEP
Transcript:
Dr. Uriel R. Felsen:
The really nice thing about PrEP coverage at this point is that it has a grade A recommendation from the US Preventive Services Task Force, the USPSTF. And so, because there’s a grade A recommendation for it, all insurances are required to cover it without any contributions from the patient.
And for those who are uninsured, there are a lot of access programs through the drug companies themselves, and some states also have an assistance programs. So pretty much anyone who is interested in being on Prep should have minimal financial barriers to being able to get it. At this point.
Starting PrEP
Transcript:
Dr. Raffaele Bernardo:
Not all forms of PrEP are approved for all types of sex. So it’s important to get a sense of who your patients are, who they’re having sex with and what body parts they’re using to have sex. That’s also important when you talk about testing for sexually transmitted infections, you want to make sure that you’re offering comprehensive testing. And this includes three site testing, perhaps for gonorrhea and chlamydia, again, depending on body parts that a patient may use to have sex. For example, oral pharyngeal swabs, rectal swabs which can be self-collected by the patient and or vaginal swabs, which could also be self-collected by the patient or urine sample, for example.
And then we offer blood work for things like HIV, for example, to make sure that the patient at baseline is not living with HIV, we do testing for syphilis and various forms of hepatitis. But most importantly, we have to test for the preexistence of hepatitis B. And the reason is because some of these medications do have activity against hepatitis B, particularly Truvada and Descovy. And so it’s very important to determine whether or not somebody may have an occult hepatitis B infection, because if you do start one of these oral forms of PrEP and then stop, you can actually cause a rebound hepatitis b viremia, and potentially could cause fulminant liver failure. So that definitely wants to be excluded.
One of the things that I think also many offices have implemented as well, which is one of the things for example, we do is same day starts for PrEP. So actually having patients, for example, leave with a prescription, or even a sample in hand to get started the same day, we find that that often helps with adherence. So some offices do have the availability of doing point of care testing for HIV. There is a slightly longer window period for many of these point of care tests, but if you exclude an acute HIV infection clinically so, people who come in without any recent flu, like syndromes, for example, fevers, chills, swollen lymph nodes rash, etc, and their point of care for HIV is negative, you can actually even start same day PrEP, particularly the oral forms of PrEP.
Tips for PrEP Adherence
Transcript:
Dr. Jonathan Shuter:
So I think that’s an idea to introduce really early to the patient that these things that pills require one pill every day. Patients have to be reliable and consistent with tha,t and the injectable, they have to show up every two months and get their injection. Otherwise it’s not going to go well. So I think that that’s a good message to start with.
Dr. Raffaele Bernardo:
So when it comes to talking about adherence, trying to really get a sense of what those barriers might be to adhere to these medications, because it might help you steer the conversation toward one medication or another. I’ve had patients who have had concerns about disclosure. They have roommates, or maybe they live with family, and they’re worried about having a pill bottle with the label of these medications lying around the house. We talk about things to do there. But that might be a candidate, for example, for Apretude, coming into the office for an injection every other month rather than storing medications at home, just as an example.
For me, I would say, the majority of the patients, the community that I do serve is a largely a younger population. So a lot of these individuals aren’t on medications for anything else. And now, all of a sudden, you’re entrusting them to take a pill every day. And so one of the big things that comes up during follow-up appointments is adherence, and not because they want to miss their medication. They just forget, because it hasn’t been part of their daily routine to take a pill every day.
So one of the things we talk about are strategies to remember. We talk about setting daily reminder alarms on their cell phones, for example, or I tell them to put their pill bottle next to something that they will reach for every morning, for example, like their toothbrush or their coffee machin,e just to help with adherence. But I think the one most common thing that I will hear from patients in terms of quote unquote issues with PrEP is just remembering to take their pill.
And, conversely, conversely, I do have a handful of patients that have lots of other medical comorbidities, and they have the other problem. They develop what we call the medicine pill fatigue. So now you’re kind of inundating them with another pill they have to take every day, and so it becomes a similar but not so similar conversation. So both ends of the spectrum.
Dr. Jonathan Shuter:
And, needless to say, for for folks who are on their 1st chronic medicine, we shouldn’t assume that they know how to get a refill or know what a refill even is. They should leave the clinic or your office with a phone number to call if they’re having problems, if they lose their pills, if they have questions about it, because if you don’t give them that and they have a problem, they’re not going to know what to do if they aren’t. They haven’t been trained in the medical system already.
Raffaele Bernardo:
One of the other strategies I mentioned to patients is, I will often offer them if I have available, or I’ll tell them to go pick one up online, is a little pill key chain, and I will tell my patients to keep one or two, I like to call them emergency pills, on them, put it on their backpack on their keychain. So, for example, let’s say it’s a night out, they spend the night at a friend’s house, or whatever the case is, they go to work the next day. They forget, but they have one or two extra pills on them to just sort of take in the event that they forget.
Jonathan Shuter:
The more strategies you offer, the more likely they are to adhere. So so, you know, I think a keychain thing, a pill box, an app, good counseling. All of those things are important, and they should be piled one on top of the other.
Stopping PrEP
Transcript:
Dr. Raffaele Bernardo:
So people’s situations change all the time. There may be a change in one’s perceived risk for HIV infection. So people come on and off PrEP all the time. But it’s important that this is done under the guidance of a provider for a few different reasons. One is, you sort of want to remind the individual that if they do stop PrEP, there is going to be, if they do engage in any risks, any sexual activities or intravenous drug use where they could be exposed to HIV, that they no longer have that medication in their body. And so an alternative form of HIV prevention should be used.
The second thing is, you again want to make sure that you’ve at least addressed the hepatitis B thing at some point, because, again, if there is a missed underlying hepatitis B infection, by stopping these medications abruptly, you can cause a viral rebound, hepatitis B viremia, and potentially fulminant liver failure. For those people who are incidentally found to have chronic hepatitis B, they do have to stay on treatment, at least in the beginning, until they are sort of staged and determine whether or not they need ongoing medication. So we’ll typically narrow them from Truvada, which contains tenofovir and emtricitabine to just tenofovir.
Dr. Uriel R. Felsen:
I think there’s one other special consideration, which is the folks that are that are on the injectable, for when they want to come off, because it’s a long-acting injectable, and the idea of stopping it would be to sort of let the drug levels peter out. But of course, during that period when the drug levels are petering out, you have some amount of of the medication in you, but not necessarily enough to offer protection. And so there is a small risk during that period, if somebody was to acquire HIV, that their strain of HIV that they’ve acquired could become resistant to the cabotegravir. So some people in that scenario have opted to start an oral medication, one of the oral PrEP options, while the cabotegravir is sort of petering out from their system.
Dr. Raffaele Bernardo:
And that’s particularly important, because the resistance mutation that occurs sometimes with cabotegravir renders a lot of these single tablet regimens we use to treat HIV ineffective. So not to say that you couldn’t treat somebody now living with HIV. But your options will be somewhat limited. So that’s a great point, thanks, Dr. Felson for bringing that up.
Recorded on September 30th, 2024 at 8 pm ET

PrEP in Complex Care: Special Populations and What’s Next
PrEP in Complex Care: Special Populations and Long-Acting Innovations
Short videos. Trusted facts.
With Dr. Jonathan Shuter, Dr. Uriel Felsen, Dr. Raffaele M. Bernardo, and Dr. Rasika Karnik
- PrEP for patients whose primary HIV risk is injection drug use
- Pregnancy and PrEP
- The Future of PrEP
- View the entire webinar here
PrEP for patients whose primary HIV risk is injection drug use
Transcript:
Dr. Uriel R. Felsen:
PrEP is for anyone that isn’t already living with HIV, and is at risk for acquiring HIV. So there are some ways to think about, some populations who may be more at risk for HIV. But I think the most important take home point for everyone to come home, you know, everyone who’s watching this to understand, is that it’s really for anyone that doesn’t already have HIV, and that is interested in protecting themselves from acquiring HIV, either through sex or through intravenous drug use.
Pregnancy and PrEP
Transcript:
Dr. Raffaele Bernardo:
So there are currently three medications that are FDA-approved for HIV pre-exposure prophylaxis.
Two of these medications come in the form of an oral tablet that’s taken once daily, and the third is actually the first long acting injectable for HIV pre-exposure prophylaxis. But all three are FDA-approved, and all three, as long as they’re taken as prescribed, are highly effective at preventing HIV infection. The two tablets are single fixed-dose combination tablets of two different medications of the brand names. One is Truvada, the other is Descovy, and the long acting injectable goes by the brand name Apretude. Apretude is given one month back to back for the first two months, and then every other month thereafter.
Dr. Uriel R. Felsen:
It’s important to remember that there are three choices, but not all choices are necessarily for all different folks. There’s an option, anybody that’s interested in PrEP, there is an option. Dr. Bernardo mentioned Descovy and Truvada. Both of them contain tenofovir and emtricitabine, but they contain different formulations of the tenofovir.
And currently, it’s really Truvada that is approved for cis men, cis women, and transgender men and transgender women, whereas Descovy is actually not approved for HIV prevention for anyone that’s at risk for acquiring HIV through vaginal sex. So that would be for cis women or potentially trans men.
The Future of PrEP
Transcript:
Dr. Jonathan Shuter:
These medications are extremely well tolerated. So almost anyone who puts any new pill in their mouth and swallows it could get some nausea. So there is, you know, a certain incidence of nausea and GI upset, associated with the two oral preparations. There were larger earlier concerns with the potential for renal effects and for bone effects with the tenofovir-containing preparations which are both of the oral medications. But most of those fears and concerns have been allayed by the collective experience that that significant renal toxicity or bone toxicity are rare.
And so those are really the common side effects with the pills. With the injection, it is basically what you would expect. With the injection, they get injection in site pain, and it is rare that that is severe enough that it causes discontinuation of the medicine, and that tends to get less with subsequent injections.
Dr. Raffaele Bernardo:
I’ll add, with the nausea that’s occasionally seen, almost always is self limiting, and within a week or so of daily use, the nausea actually goes away without any particular intervention. So I will often counsel my patients and say, while it’s rare, you may experience some nausea in the first few days. If it’s not too uncomfortable, keep taking your pill daily, and almost invariably the nausea self resolves within a couple of days when it happens. But to Dr. Shuter’s point, these side effects are typically very rare.
Recorded on September 30th, 2024 at 8 pm ET

Ready to start PrEP? Some Quick Videos
Where to get PrEP
Transcript:
Dr. Raffaele Bernardo:
I think the first place to go is if you feel comfortable, is having a conversation with your primary care provider, a point of contact, somebody, presumably, you know, and trust somebody you can probably have easy access to
if you feel comfortable having these conversations, you can easily bring up this conversation with your primary care provider. Now, having said that, more often than not, I’m getting patients in my office, for example, who are coming to me specifically for sexual health because they don’t feel comfortable having these conversations with their providers. So one of the things you could do if you aren’t comfortable is to go online, see if there are any sexual health clinics nearby. If there are any infectious diseases offices nearby. There are plenty of online resources where you can search for providers.
Now, if there was an issue, for example about disclosure, or perhaps being seen in public, there are also several online services as well that can help set you up for PrEP. These are still run by healthcare providers who will perform an intake visit, and will check in every three months or so, and still require testing. But it is an alternative to in-person visits, if there is any limitation in that regard.
So I would start with your PCP. If you already have an established relationship. If not, and you feel more comfortable, you can do some searching online looking for a sexual health clinic or an infectious diseases office nearby. Or there are several online services as available as well, which are accessible through apps as well, that you can download through your phone.
One of the other one of the other options as well, is, if you do find a local provider or your provider that you’ve already established with, they may offer the opportunity to do telemedicine services as well. So what’s nice about telemedicine is that you can obtain medical care without leaving home. There are some limitations. You, as a patient, need to be located in this, in in the state that your provider is licensed. But it is an option to expand availability if distance is an issue
What to Expect at Your Doctor Visit
Transcript:
Dr. Uriel R. Felsen:
At your first appointment, where you might be speaking to a provider at PrEP, I’m sure that the provider is going to have questions for you about what kind of sex you have, who you’re having sex with, to try to get a sense of what is your risk for HIV, and how can, and whether PrEP might be a good option for you to protect yourself against HIV.
It’s also going to be important to know just more about you as a person, and whether you have other medical issues, because that might have an impact on which PrEP medication is appropriate for you.
So a lot of questions about yourself, and about your sex life. Some questions about your about your medical history.
One of the most important things is to have an HIV test before you start PrEP. To make sure that you don’t already have HIV. Some of the other tests that that are going to be done are looking for other sexually transmitted infections, just routine care, so gonorrhea, chlamydia, syphilis. Some of these infections might cause infections of the genitals, but sometimes they can also cause infections of the throat or infections of the rectum. So your provider may be asking you, maybe collecting specimens, you know, from your throat a throat swab as well as a rectal swab. Rectal swabs are things that patients can even do by themselves. It’s really just a q-tip where you get a little swab in the area and it gets sent off to the lab. So some some blood tests, some swabs. We talked about syphilis, which would be a blood test. And another important one is going to be hepatitis B.
So people that are starting on PrEP, we need to know whether you have hepatitis B or not, because some of the medicines for PrEP will also treat hepatitis B.
And so, if there is a small risk, that if somebody with hepatitis B were to stop their PrEP medication, it could cause a flare of the hepatitis B virus, which is something that affects the liver. So there’s just some routine labs that are going to be done at your 1st visit, along with getting a thorough history.
Paying for PrEP
Transcript:
Dr. Raffaele Bernardo:
So one of the messages I like to convey to both patients and and providers, healthcare providers who may be offering PrEP services, that anyone who needs PrEP, whoever wants PrEP, can get PrEP, and finances should never be an issue. Whether you’re insured, uninsured, underinsured, there’s a mechanism to get some form of PrEP.
Now, the USPSTF, that’s the United States Preventative Services Task Force. This is the Federal organization that makes recommendations for certain screening tests – for example, when we’re supposed to get our colonoscopies, our mammograms, pap smears, etc. That same organization has given PrEP a grade A recommendation.
Now, this is important for many reasons. But one reason in particular is that any recommendation that’s given a grade A is supposed to have, those services are supposed to be provided to patients with no cost sharing on the side of the patient. In other words, if a patient wants or needs PrEP and is insured, they should have no out-of-pocket expense when they go to the pharmacy to pick up these medications.
If a patient is under or uninsured, there are programs that are available to assist people in obtaining these medications
For people who do have coverage, but, let’s say, have a large out-of-pocket, the pharmaceutical companies also have what’s referred to as Copay assistance. So let’s say your insurance does cover PrEP whatever form it is but you have a large out-of-pocket. These pharmaceutical companies do offer Copay assistance up to a certain amount per year, which very often will cover the bulk, if not the entire, out-of-pocket cost for the year. So, in other words, ability to pay should not be a limitation for getting HIV pre-exposure prophylaxis. It is available at little to no cost in one way, shape or form.
Recorded on November 4th, 2024 at 8 pm ET

Already Using PrEP? Some Quick Video Tips
How Soon is PrEP Effective?
Transcript:
Dr. Raffaele Bernardo:
We do have some data that show that for Truvada in particular, it does take about 7 days of continuous use before it achieves levels within rectal tissue that are considered protective against HIV. In vaginal tissue we think this is closer to 3 weeks or 21 days or so. In my practice, I extend that data to include Descovy, although there’s probably a difference between the two. But just for precautionary measures, we typically will also generally recommend the same amount of time, 7 and 21 days, with the rectal and vaginal tissue respectively. For penile tissue, oropharyngeal tissue, or the throat, for example, we don’t have as good data, but largely, I would recommend closer to a 2 or 3 week mark in that regard. But the data that we do have, rectal tissue 7 days, vaginal tissue, approximately 21 days.
For injectable Apretude we believe there is about a 7 to 14 day window before the drug achieves protective levels in the blood after your first injection, so I often will inform my patients, who are already on some form of oral PrEP to continue their oral PrEP for approximately 14 days after their first injection, to ensure that the injectable Apretude has reached levels that are protective against HIV.
Tips for Remembering to Take PrEP
Transcript:
Dr. Uriel R. Felsen
The effectiveness of pre-exposure prophylaxis is directly correlated to how well you take it. Meaning, are you adherent to it? Are you taking it as it’s prescribed every day? And so a lot of people have come up with ways to integrate taking a medication into their daily routine. Some people will you know, decide to take it every, the same time every day, and so they’ll sort of attach it to something that they do on a routine basis, like brushing their teeth at the same time every day. Keep their pill bottle there. Other people might use a pill, might have a medication pack that they carry around with them, and set an alarm on their on their calendar or on their smartphone to remind them every day.
Dr. Jonathan Shuter:
But you have to also anticipate other situations. What are you going to do when you go on vacation? The time to think about it is not when you’re running to the gate in the airport. The time to think about that is the day before. What should I do? Where should I pack this?
Or, if you’re going to go sleep at a friend’s house for the night and be out of your house for 24 hours. How can you take the pill along in a way that works for you, because if you don’t think of those things in advance, they’re not going to happen, and your adherence is going to fall down, and when PrEP fails, it is because patients don’t take their pills right. So please give that some thought. If you’re contemplating starting prep, or you’re on it now, think about how to stay on it really, really, reliably, over the course of time.
What if you Miss a Dose
Transcript:
Dr. Jonathan Shuter:
This medicine only works if you take it and take it as you’re supposed to. But what happens if my routine is to take it at 8 am, every morning. And then one day at dinner time, I realized I didn’t take it, I didn’t take my 8 am dose. That’s scenario number one.
Scenario number two is, what if I miss a whole day? You know I missed my Thursday dose? And here’s Friday, and am I still protected? And what should I do? Should I double dose? Or what’s the correct approach?
Dr. Uriel R. Felsen:
That’s a great question. And you can imagine that this comes up all the time, and nobody’s perfect, and nobody is going to be expected to take their medication at the exact same time every day, 365 days a year. So this definitely comes up and we have to have real world expectations of our patients. And so the idea is, you want to do the very best that you can. So let’s say you take your pill. Let’s say you’re on Descovy or Truvada, and you take your pill every day at the same time at 8 am.
And come that evening, you realize you haven’t taken it yet? Go ahead and take it, and that’s it, you’re going to be just fine. You’re within the same 24 hours. It’s it’s just fine. You’ll be able to take your next pill at 8 am the next day without having to worry about it.
That would be for the first situation that you said.
If you entirely missed a day, don’t double up on your meds. If you missed your Monday dose, and now you wake up on Tuesday and said, Oh, my God! I forgot to take it. Take your Tuesday dose, forget about the Monday dose. It should be all right. Everyone is, you know, the idea is to take it as consistently as you can, and we want to make sure that you take it almost every day. But if you miss a day. It’s not worth the potential risk of having too much medication on board by doubling up that day.
Stopping or Restarting PrEP
Transcript:
Dr. Raffaele Bernardo:
So obviously things, life, circumstances, change, relationships come and go, and so can PrEP. People can stop and start PrEP as they feel is necessary. However, we do recommend it is done under the guidance of a healthcare provider, for a couple of reasons.
In terms of discontinuing PrEP. Dr. Felsen had alluded earlier about checking for underlying hepatitis B infection prior to starting PrEP. The same is true when you stop PrEP. If it was missed initially and again, just to remind everyone, the reason is because these oral forms of PrEP do have activity against hepatitis B as well.
And if an infection is missed, and these oral forms are stopped, you can actually have a rebound infection and can develop fulminant liver failure. And so we do have to screen, if it wasn’t screened for initially. If someone does have chronic hepatitis B, they do need to remain on at least one form of hepatitis B medication that that individual can discuss with their provider
In terms of restarting. PrEP, again, similarly, things change and people can definitely restart. However, prior to restarting prep, you do need an HIV test to make sure that you are, in fact, HIV-negative before restarting PrEP. So you should never just keep the pills at home, decide to stop for a month or two and then pick it up, you know two, three months down the road without discussing with the healthcare provider, because those tests do need to be repeated, and to make sure we aren’t missing anything.
When it comes to the injectable form of proper aptitude, there is an additional concern. Apretude does have a very long what we refer to as a tail, meaning that after the injection it does take a while before the medication is completely eradicated from the body. And the reason this is concerned is because if someone does have an HIV exposure during this quote unquote tail period, they may still get infected, they may still get HIV. But now, because you have that low level drug available in your system, the HIV virus can become resistant to that medication, and not that we couldn’t treat the HIV infection. But we have to be a little bit more creative with our medications.
So that’s an additional nuance in terms of starting and stopping PrEP when it comes to the injectable. Not that someone would do this at home, since it has to be done in the healthcare provider’s office, but something to keep in mind. If you stop injectable PrEP. If you feel that there may be a potential risk for HIV acquisition to make sure you’re using some other form of HIV prevention like condoms, for example, until you are able to return to your doctor’s office to discuss restarting injectable Apretude.
Pregnancy and PrEP
Transcript:
Dr. Uriel R. Felsen:
So Truvada is safe in pregnancy, where one partner is living with HIV and the other partner is not living with HIV, and sometimes a couple like that might be trying to conceive, and so Truvada is an option in that situation to help prevent acquisition of by the person who’s not living with HIV, and also to protect the fetus.
The injectable is relatively new. We don’t really have enough information about cabotegravir in pregnancy. At this point, if you are on Cabotegravir and you become pregnant, you’d want to discuss with your provider the options of either staying on it or potentially switching to Truvada. That would be a discussion to have.
But people who are on Truvada can continue that through pregnancy.
Dr. Raffaele Bernardo:
So the two things I was going to add, one is right, so these are medications like Truvada, for example, that we’ve been using for a very long time, particularly with people living with HIV who get pregnant. So we have a lot of good data showing its safety profile in the setting of pregnancy. The other thing I will add to what Dr. Felsen mentioned is that while Descovy is safe in pregnancy, it typically is not, or it should not be a medication that we would be giving for HIV pre-exposure prophylaxis in somebody who is capable of getting pregnant. And the reason is because it is not FDA-approved for people who engage in receptive vaginal sex. So again, while it is safe in terms of the fetus, it is not a medication that somebody in that situation would be prescribed prior to getting pregnant. Presumably.
Recorded on November 4th, 2024 at 8 pm ET

Curious About PrEP? A Webinar for Patients
Curious about PrEP but not sure where to begin? This webinar breaks down everything you need to know—from how PrEP works and how effective it is, to the different medication options, how to get a prescription, and ways to pay for it.
You’ll also get tips for taking it consistently and learn what to expect if you ever decide to stop. Whether you’re just starting to explore or ready to take the next step, this video can help you decide if PrEP is right for you.
Get quick answers to common questions, from doctors who specialize in PrEP care.
Recorded on November 4th, 2024 at 8 pm ET
Faculty: Jonathan Shuter, MD, Uriel Felsen, MD, and Raffaele M. Bernardo, DO
Full Webinar
Transcript Summary:
Key Highlights:
- What is PrEP? PrEP (pre-exposure prophylaxis) is a medication taken before potential exposure to HIV to prevent infection. It’s recommended for anyone at risk—including people who are sexually active or who inject drugs.
- Effectiveness: When taken as prescribed, PrEP is over 99% effective at preventing HIV.
- Options: There are three FDA-approved PrEP medications—two daily pills (Truvada and Descovy) and one long-acting injectable (Apretude).
- Getting Started: Patients can get PrEP through their primary care provider, local sexual health clinics, or telehealth services. The first visit typically includes a conversation about sexual health and some lab tests.
- Adherence Matters: PrEP only works if it’s taken consistently. Strategies like setting phone reminders or linking the pill with a daily habit can help.
- Side Effects & Safety: Side effects are generally mild and temporary. Truvada may affect kidney or bone health, but this is rare and reversible. Truvada is also safe during pregnancy.
- Access & Cost: PrEP is covered by most insurance plans with no out-of-pocket cost, and assistance programs are available for those who are uninsured or underinsured.
- Empowerment: Choosing PrEP is a proactive step in managing sexual health—not just HIV prevention—and should be seen as part of a broader wellness plan.
Final Takeaway: PrEP is a powerful, underutilized tool in HIV prevention. With multiple options, minimal side effects, and widespread availability, anyone at risk should feel empowered to talk to their provider about whether it’s right for them.
For more information, visit the PrEP for Patients Resource Center at pcmedproject.com or explore CDC materials at https://www.cdc.gov/hiv/prevention/prep.html
Transcript:
Moderator: Hello, and welcome to our webinar for people interested in learning more about PrEP medication that can lower your risk of HIV infection. Tonight we’re going to go over the basics of PrEP. What is it? How it works, where to get it, and how to use it?
And we’ll answer any questions you might have. Feel free to put your questions in the chat.
And doctors, if you would please be so kind as to introduce yourselves.
Dr. Jonathan Shuter: So maybe we should go in alphabetical order. So, Dr. Bernardo, why don’t you go first?
Dr. Raffaele Bernardo: Sure. Good evening, everyone. My name is Dr. Bernardo. I am an internist and an infectious disease specialist by training. I’m currently the medical director for a comprehensive LGBTQ plus program located in Northern New Jersey. And I’m excited to be here tonight.
Dr. Jonathan Shuter: Thanks, and Dr. Felsen.
Dr. Uriel R. Felsen: Hi, I’m Uri Felsen. I’m an infectious diseases physician at Montefiore Medical Center in Albert Einstein College of Medicine, and I work with people who are living with HIV and people who are at risk for HIV.
Dr. Jonathan Shuter: And Hello! I am Jonathan Shuter. I’m an infectious disease physician also at Montefiore Medical Center, and the Albert Einstein College of Medicine. I think I’m the oldest person on in this group. And saw my very first patient in 1985, with HIV. And I’ve been involved in HIV medical care going on 40 years.
So I guess we should get started. And let’s start with the basics. Let’s start by asking and answering the question, what is PrEP. And I think that I will send that to Dr. Felsen for the first answer.
Dr. Felsen: Thanks, Dr. Shuter. So PrEP stands for pre-exposure prophylaxis. And the idea is that it is a medicine that you get into your body ahead of time to protect yourself from the risk from acquiring HIV. So this is a medication for anyone who’s not already living with HIV, who may be at risk for HIV, and it’s a medicine that you take to protect yourself from acquiring HIV down the line.
Dr. Shuter: Great. And so I’d like to just dive into that a little bit a little bit more. So. Who is it that should consider using PrEP.
Dr. Felsen: So, you know, PrEP would really be great for anyone who is not currently living with HIV, who wants to protect themselves from it. So some of the people. So anyone who is sexually active should be talking to their provider about PrEP. That’s the recommendation from the CDC. And people who inject drugs as well, should also consider protecting themselves from HIV using PrEP. And can talk to their providers about that.
Dr. Shuter: Great. So I appreciate that answer, and I think if I might even express it more tersely, and say that that anyone who is at more than zero risk for HIV can consider PrEP.
It’s not necessarily for everybody, but a corollary to that statement is that someone who is at zero risk for HIV probably shouldn’t take PrEP. There’s probably no reason to put those chemicals in your body if you’re at zero risk. But assessing whether you are at any risk or zero risk is an equation that you might want to work out with your physician.
Dr. Bernardo: One of the things. I’ll add, Dr. Shuter, that, I think, is also helpful, too, in an effort to get a sense of someone’s perceived risk or actual risk for HIV is to think about the partners that that individual may be having sex with. If they know the HIV status of the partners that they are engaging in sex with, or, for example, if they’ve had a bacterial sexually transmitted infection in the past before, like, for example, syphilis, gonorrhea or chlamydia.
And the thought behind that is in reality, if you’re at risk for one sexually transmitted infection, there is a possible risk for another, and so a good gauge about whether a good gauge for whether or not someone may benefit from PrEP would be to think about history of bacterial, sexually transmitted infections in the past.
Dr. Shuter: Okay. So at this point, we’ve established that there is a treatment option for or there are treatment options for someone who is at risk for HIV, and wants to take measures to prevent acquiring HIV. How well does it work? Let’s let you take that one, Dr. Bernardo.
Dr. Bernardo: Sure. So we have very, very good data that show that HIV preexposure prophylaxis, regardless of its form, is incredibly effective at preventing HIV assuming an individual is taking the medication as prescribed.
We’re looking at 99% plus effectiveness at preventing HIV. Now, there’s a very good correlation between adherence and efficacy, meaning that if you take the medication it works. If you don’t take the medication, it doesn’t work. And so that’s really the driving point here to be made.
Dr. Shuter: So maybe we could now get into the different choices that one might have as far as PrEP medications. Dr. Bernardo.
Dr. Bernardo: Sure. So there are currently three FDA-approved medications for HIV pre-exposure prophylaxis. Two come in the form of pills. Each of those is taken as one pill once a day every day. Whether or not you’re having sex. Those two pills go by the brand names of Discovy and Truvada, and they’re both single tablets that are taken once a day every day.
The third option is the first long acting, injectable medication, called Apretude. Apretude is given in a provider’s office healthcare Provider’s office. It’s given as an injection during one month, one month, two, and then every two months thereafter. So it might be a good option for some people. We’ll talk a little bit later, as far as perhaps, who might benefit from one form over the other. But currently these are the 3 FDA approved medications that are available for HIV pre-exposure prophylaxis.
Dr. Shuter: Okay? And Dr. Felsen, I want to just bring up this question. We are talking to an audience tonight of people who may have never taken a medication regularly before, and aren’t comfortable, or might not be comfortable with the nuts and bolts of starting on a medicine and continuing on it. So might you have any words of wisdom about that about someone who’s starting on a medicine, and might not be accustomed to being on medication over the long term.
Dr. Felsen: Yes, it’s a big change. And for folks that aren’t used to taking a medicine every day, that might be something really new and something to get used to, and as Dr. Bernardo mentioned, you know the effectiveness of pre-exposure prophylaxis is directly correlated to how well you take it. Meaning, are you adherent to it? Are you taking it as it’s prescribed every day? And so a lot of people have come up with ways to integrate taking a medication into their daily routine. Some people will decide to take it every the same time every day, and so they’ll sort of attach it to something that they do on a routine basis, like brushing their teeth at the same time every day. Keep their pill bottle there. Other people might use a pill, might have a medication pack that they carry around with them, and set an alarm on their calendar or on their smartphone to remind them every day. There are lots of different strategies that people have used to remember to do it every day, but it is true that for many people who are starting PrEP, this might be the 1st time that they’re taking a medication every day. So it’s definitely something to be considered.
Dr. Shuter: Yes. And I think that that’s a great point. And and you know, one of the most consistent findings in all studies that PrEP that have been done so far is that the Achilles heel of PrEP. When it doesn’t work, it is almost always when a patient isn’t taking it. Well, so
I’m stating the obvious here, but I’m going to state it, anyway, that that medicine that sits in a bottle in your medicine cabinet and doesn’t go into your mouth and get swallowed doesn’t work. So if this is a decision that one takes, then that it is a decision that one should really stick with and follow the instructions.
And let me just ask another simple question. Either of you jump in, but we’re going to continue along, not assuming that people know how to take medicines chronically. What do you do when there’s only two pills left in the bottle.
Dr. Felsen: You have to make sure to stay on top of getting refills through your physician or your provider, whoever is prescribing PrEP. So PrEP is a medication that will need to be prescribed by a provider, and you’ll get it through a pharmacy. And most likely it’s going to be distributed on a dispensed to you on a monthly basis. And so, as that month’s supply is coming to an end, it’s important to look at your pill bottle and see, is it written on there that there’s any more refills remaining? And if there are, call up your pharmacy, ask them. Let them know that you’re due for a refill, and you’re ready to either pick it up or have it delivered. And if there are no more refills coming, you need to make sure to call your provider so that they can send in the next set of refills for you.
Dr. Bernardo: One of the things I’ll add as well is, many pharmacies also have the option for automatic refills as well, so they’ll keep track of when your last dispense was for your medication, and once they realize that you’re getting down to the last few days of medication, they’ll send an alert via text, or perhaps through a pharmacy app to let you know that you probably are due for a refill, and they’ll ask if you want the medication refilled
So that can serve as an additional reminder. So one of the things I do tell my patients is, if you think you might have issues remembering to ask for refills, see if your pharmacy has this service available. You sign up once and you’ll get reminders as you get toward the end of your month supply of medication. But to Dr. Felsen’s point, once you are reaching that three month mark, and you are due for additional refills, iIt’s important to reconnect with your provider, because you will also require repeat HIV testing at that point as well.
Dr. Shuter: Yes, and so a clear message here is that the patient stands at the center of a healthcare team that includes a physician or other prescribing provider and a pharmacist, and if things come up in the course of taking PrEP. If you lose your medicine, if there’s a fire and your medicines burn up if any kind of accident happens, then the people to call are those people because there are usually remedies for those kinds of urgent situations.
So moving on. If someone were interested in starting in prep, how does that person go about getting it? Who do you call, or who do you, Google? Or with whom do you set up an appointment.
Dr. Bernardo: So I can. I guess I can. I can start. I think the first place to go is if you feel comfortable, is having a conversation with your primary care provider point of contact, somebody, presumably, you know, and trust somebody you can probably have easy access to if you feel comfortable having these conversations, as you should. You can easily bring up this conversation with your primary care provider. Now, having said that, more often than not, I’m getting patients in my office, for example, who are coming to me specifically for sexual health because they don’t feel comfortable having these conversations with their providers. So one of the things you could do if you aren’t comfortable is to go online, see if there are any sexual health clinics nearby. If there are any infectious diseases offices nearby. There are plenty of online resources where you can search for providers.
Now, if there was an issue, for example about disclosure, or perhaps being seen in public, there are also several online services as well that can help set you up for PrEP. These are still run by healthcare providers who will perform an intake visit, and will check in every 3 months or so, and still require testing. But it is an alternative to in-person visits, if there is any limitation in that regard.
So I would start with your PCP, if you already have an established relationship, if not, and you feel more comfortable, you can do some searching online looking for a sexual health clinic or an infectious diseases office nearby. Or there are several online services as available as well, which are accessible through apps as well, that you can download through your phone.
Dr. Shuter: Right. So I I do want to emphasize that last point that we all work in urban centers where usually transportation to various provider settings is fairly easy. But we may have people viewing this webinar who live in rural settings, and it could be a 60 mile drive to get to their providers. So I think you mentioned this already. But might you say another word or two about availability of telehealth, and whether that’s a viable way of securing access to PrEP.
Dr. Bernardo: Absolutely so. One of the other options as well, is, if you do find a local provider or your provider that you’ve already established with, they may offer the opportunity to do telemedicine services as well. So what’s nice about telemedicine is that you can obtain medical care without leaving home. There are some limitations. You, as a patient, need to be located in the state that your provider is licensed. But it is an option to expand availability if distance is an issue.
We in our office do provide telemedicine for PrEP as well. We do recommend that patients come in at least once a year to be seen in person, because I think and I’m sure we’ll discuss this a little bit later, PrEP. Is more than just HIV prevention. And there’s some other topics and vaccines and things like that that we do prefer to talk about in person. But when it comes to PrEP, we do offer the opportunity to do telemedicine as well, and it has improved access to care.
Dr. Shuter: Okay, so let’s let’s move along here. You’ve identified the provider that you want to speak to about PrEP. What does someone who is going to start PrEP. Or is considering it? What should they expect at the initial doctor visit? Maybe Dr. Felsen can chime in on that.
Dr. Felsen: Sure. So you know when, at your first appointment, where you might be speaking to a provider about PrEP, I’m sure that the provider is going to have questions for you about what kind of sex you have, who you’re having sex with, to try to get a sense of what is your risk for HIV, and how can and whether PrEP might be a good option for you to protect yourself against HIV. It’s also going to be important to know just more about you as a person, and whether you have other medical issues, because that might have an impact on which PrEP medication is appropriate for you.
So a lot of questions about yourself, and about your sex life. Some questions about your
about your medical history. And you’re also going to – one thing that Dr. Bernardo was mentioning that is another challenge in telehealth is the fact that there are some routine labs that you’re going to get during your first provider visit. So remember that PrEP is really for anyone that’s not already living with HIV. So one of the most important things is to have an HIV test before you start PrEP, to make sure that you don’t already have HIV.
Some of the other tests that are going to be done are looking for other sexually transmitted infections, just routine care, so gonorrhea, chlamydia, syphilis. Some of these infections might cause sort of infections of the genitals, but sometimes they can also cause infections of the throat or infections of the rectum. So your provider may be asking you, maybe collecting specimens, you know, from your throat a throat swab as well as a rectal swab. Rectal swabs are things that patients can even do by themselves. It’s really just a Q-tip where you get a little swab in the area and it gets sent off to the lab. So some some blood tests, some swabs. We talked about syphilis, which would be a blood test. And another important one is going to be hepatitis B. So people that are starting on PrEP, we need to know whether you have hepatitis B or not, because some of the medicines for PrEP will also treat hepatitis B. And so, there is a small risk, that if somebody with hepatitis B were to stop their PrEP medication, it could cause a flare of the hepatitis B virus, which is something that affects the liver. So there’s just some routine labs that are going to be done at your first visit, along with getting a thorough history.
Dr. Shuter: Yes, so just to just to summarize, medical issues in the background. That could be important. Particularly, if there is significant renal or kidney disease, and also a history of hepatitis B, those would be of some importance.
Dr. Bernardo, I’m going to ask you to answer this question in a second, but I will also give my poor man’s answer to it before I ask you, what if a person who’s thinking about PrEP is embarrassed to go to the doctor? So my routine answer is that I’ve been a doctor a long time, and there’s nothing you could tell me that I haven’t heard, you know, many, many times before, and probably way more embarrassing than what than what you’re going to tell me. But I’d like to hear your insight. What would you advise? Someone who, where the impediment is embarrassment.
Dr. Bernardo: Sure. One of the things that I often tell my patients is that most people probably want to have these conversations, and probably many providers are ready to have them. But it’s always awkward who’s going to start the conversation, so I generally tell my patients to be open and honest with their providers, because these are conversations that are very important. They are on most people’s minds when they come into the doctor’s office.
And we try to normalize the conversation, because I often say to my patients, Look, your overall health is not just about your physical health. Right? You come in. You get vitals. We check your blood pressure. We do blood work, we do. X Y and Z. But your overall health is also about your mental health. It’s about your sexual health, and each one is just as important as the next. And so I do try to normalize these conversations. I often tell my patients these are routine questions that I often will ask of all, and if I will ask all of all of my patients, and if my patients don’t feel comfortable bringing them up, I will bring it up myself. And more often than not, when I bring up those questions they also start opening up to me and say something to the effect of you know I, I wanted to ask you those questions, but I was, I was nervous. I wasn’t sure if you were prepared to answer them.
And so I try to normalize these conversations, and I think the more we do that, number one as providers, I think it definitely helps from the patient experience, but from the patient side of things, I think it’s important that we remember that our sexual health is just as important as the rest of our overall health.
And these are questions that you need to ask in conversations you have to have with your healthcare provider.
Dr. Shuter: Thank you, Dr. Felsen. A very, a very simple, straightforward question. We talked about what to expect at the initial doctor visit, and it sounds like there is going to be a bunch of questions and question answer session, and there’s going to be some blood draw done. When do I expect to have pills in my hand?
Dr. Felsen: So you can walk out that day with a prescription for PrEP. So as long as you know, we do want to make sure that that HIV test is negative, but you might have had been able to have a rapid test on site. And at this point, very often, even if it’s not a what’s called a rapid test that you’re seeing, you know the little line on the strip in front of you, even if it’s sent to the lab, you may have the answer by the next day. So, most providers, at this point, in the absence of any suspicion that you might already have HIV, would feel comfortable sending you out with a prescription that day.
Dr. Shuter: Great, so I hope I don’t get in trouble by saying that it’s actually faster than Amazon Prime. You go to the doctor, you will probably have, and you go to the pharmacist, you will probably have treatment in your hand that day.
Next, Dr. Bernardo. I think that the audience knows that these medicines are not necessarily cheap, and some of them are quite expensive. So how do you pay for it? Or how does it get paid for.
Dr. Bernardo: Sure. So one of the messages I like to convey to both patients and providers, healthcare providers who may be offering PrEP services, that anyone who needs PrEP, whoever wants PrEP can get PrEP, and finances should never be an issue. Whether you’re insured, uninsured, underinsured. There’s a mechanism to get some form of PrEP.
Now, the USPSTF, that’s the United States Preventative Services Task Force, this is the Federal organization that makes recommendations for certain screening tests. For example, when we’re supposed to get our colonoscopies, our mammograms, pap smears, etc. The same organization has given PrEP a grade A recommendation. Now, this is important for many reasons. But one reason in particular is that any recommendation that’s given a grade A, those services are supposed to be provided to patients with no cost-sharing on the side of the patient. In other words, if a patient wants or needs PrEP and is insured, they should have no out-of-pocket when they go to the pharmacy to pick up these medications. Now this is particularly true of the generic version of Truvada. That medication is available at no cost to people who are currently insured.
Other medications, or, for example, if a patient is under or uninsured, are available through various support programs, either locally through the city, the State, or even through the pharmaceutical company itself. There are programs that are available to assist people in obtaining these medications.
For people who do have coverage, but, let’s say, have a large out-of-pocket, the pharmaceutical companies also have what’s referred to as Copay Assistance. So let’s say your insurance does cover PrEP whatever form it is. But you have a large out-of-pocket. These pharmaceutical companies do offer Copay Assistance up to a certain amount per year, which very often will cover the bulk, if not the entire, out of pocket cost for the year.
So, in other words, ability to pay should not be a limitation for getting HIV pre-exposure prophylaxis. It is available at little to no cost in one way, shape or form.
Dr. Shuter: Thank you, and this also is for you, Dr. Bernardo. The conversation that we are having this evening has been dominated by a discussion of pills. There are two different pills available for PrEP. And it’s appropriate to spend most of our time on that, because that that is something like 99% of the PrEP prescriptions that are written in this country. But I don’t want to ignore the fact that there’s an injectable option. So I wonder if you could just say a few words about the injectable option.
Dr. Bernardo: Sure, so the injectable aptitude is the first ever long-acting injectable for HIV preexposure prophylaxis, and I think it does have some benefits over the pills, and vice versa, of course. But in terms of the pros with the injectable, one of the situations that comes up not infrequently is, for example, the issue with pill fatigue. So patients who already on several other medications and now adding another medication, it becomes daunting.
The second situation I often come across is an issue surrounding disclosure. So patients who may live with family, or, let’s say, close friends who are concerned about having a pill bottle around that may be found by whoever they’re cohabitating with. Or in the situation I think Dr. Felsen mentioned earlier. Somebody who’s new to pills, and now all of a sudden has to remember to take a pill every day, that can also be daunting as well. These have been three situations where I have found injectable Cabotegravir to be, or injectable Apretude, to be incredibly helpful.
It reduces the need to remember to take a pill every day. It helps around the situation of disclosure, since you don’t have to, you don’t have to keep a medicine bottle around the house, and it minimizes the need for additional medications you have to take every day for those who are already taking several different medications. So it is a great option.
The injectable is very well tolerated. There are minimal to. If any side effects. The big thing that occasionally we will see is injection, site pain. This is an injection that does have to be given in the provider’s office. It is an intramuscular injection, and, like was mentioned earlier. The 1st 2 injections are given back to back month one and month 2 for what we refer to as a loading dose, and then every 2 months thereafter for maintenance dosing.
So there are some people who have some injection site pain, although it isn’t limiting, for I would say, the overwhelming majority of people. And typically that injection site pain gets better with each subsequent injection. So I think injectable Apretude definitely has its place in the HIV pre-exposure prophylaxis realm for certain subsets of individuals.
Dr. Shuter: Okay. So at this point I’ve identified a provider. I’ve made an appointment. I kept that appointment. I answered all the questions, I had my blood drawn, I received the prescription. I went to the pharmacy. I have the bottle of pills in my hand.
And I’m taking the first one, so I’m very interested to know what kinds of side effects to anticipate, and whether there are any significant dangers associated with these pills or with the injectable. So, Dr. Felsen, could you address that.
Dr. Felsen: Sure. So for PrEP, all three of the options are really well tolerated. Like any medications, though, anything that you put in your body, there’s always the potential for side effects. So with both of the pill options, both of the oral options, the most common side effects are going to be gastrointestinal. So people with some GI upset usually will sort of pass. People will sort of get used to it over the first couple of weeks of being on the medication. Sometimes people have headache as well. That also usually passes
Like Dr. Bernardo mentioned for Apretude for the injectable form, by far the most common side effect is the injection site pain that he was talking about.
So as far as other side effects that one might want to know about and consider for the pills, for Truvada, the most common one, the one that people might have heard about, are that some people can have some effect on their kidney function, which is usually very mild, and your doctor, it’s something that would be recognized by checking blood tests and looking at your kidney function. And if it’s something that’s happening, if your physician or your provider finds that Truvada is affecting your kidneys, then you would most likely stop it, and at which point your kidney function would go back to where it was. So it’s reversible.
That’s with Truvada.
For Descovy, which is the other pill option, the impact on your kidney is less so. Even with people who have underlying kidney disease for whom Truvada might not be an option, Descovy might be an option. So kidney is one thing. The other thing that people talk about is bone health.
So Truvada also can decrease sort of the density of your bones. It has not been shown to be very clinically significant, meaning it’s not like people are developing new fractures. Once they start Truvada, it’s more of a lab finding or an imaging finding. And again, like the kidney function, if one were to stop the medication, the bones go back to their baseline health.
Dr. Shuter: Yes, thank you. So in summary, one could expect maybe a little bit of nausea with the pills. A bit of pain at the injection site with the injectable, and those usually get better over time.
As someone who’s been in this field for many, many years, I can say that at the outset when we began using Truvada -it’s over a decade ago already, when we started using it for PrEP – there was significant concern that kidney issues and bone issues would come up, and by and large those concerns have not materialized. And not to say that there’s no effect. But the effect that’s been observed is very, very mild, and usually reverses after you stop the medicine. So I think we have to take all potential side effects seriously. But the side effect profile of all of these medicines is very, very favorable.
Dr. Shuter: Next question, how about someone who is pregnant, or is anticipating pregnancy? What’s the track record of safety of these medications in pregnancy?
Dr. Felsen: So Truvada is safe in pregnancy and can be used, you know. Certainly there’s the situation in a zero discordant relationship. So that’s a situation where one partner is living with HIV and the other partner is not living with HIV, and sometimes a couple like that might be trying to conceive, and so Truvada is an option in that situation to help prevent acquisition by the person who’s not living with HIV, and also to protect the fetus. So Truvada is safe in pregnancy.
Cabotegravir, or Apretude, the injectable, is relatively new. We don’t really have enough information about cabotegravir in pregnancy at this point. If you are on cabotegravir and you become pregnant, you’d want to discuss with your provider the options of either staying on it or potentially switching to Truvada. That would be a discussion to have. But people who are on Truvada can continue that through pregnancy.
Dr. Shuter: Yes, so then all of that is valuable information, and I think it’s worth pointing out that, as far as Descovy and cabotegravir, Apretude, go, as far as I know, there is no worrisome safety signal with regard to pregnancy or effects adverse effects on the fetus. But what you said is true. There’s not enough data to really rely on that, at this point.
Dr. Felsen: Lots of years of experience with Truvada.
Dr. Bernardo: Right. So the two things I was going to add, one is these are medications like Truvada, for example, that we’ve been using for a very long time, particularly with people living with HIV who get pregnant. So we have a lot of good data showing its safety profile in the setting of pregnancy. The other thing I will add to what Dr. Felsen mentioned is that while Descovy is safe in pregnancy, it typically is not, or it should not be a medication that we would be giving for HIV pre-exposure prophylaxis in somebody who is capable of getting pregnant. And the reason is because it is not FDA-approved for people who engage in receptive vaginal sex. So again, while it is safe in terms of the fetus, it is not a medication that somebody in that situation would be prescribed prior to getting pregnant. Presumably.
Dr. Shuter: Right, so that probably is worth repeating. The pill Truvada is is approved for pretty much every population who would be interested in PrEP. Whereas Descovy is not
approved for those practicing receptive vaginal intercourse.
Dr. Shuter: okay. Next question. How quickly after I start does it begin to work? How soon does protection kick in.
Dr. Bernardo: So this is a this is a very important question, and not something that routinely patients bring to the table. So I think it’s important that we do discuss. So we do have some data that show that for Truvada in particular, it does take about 7 days of continuous use before it achieves levels within rectal tissue that are considered protective against HIV in vaginal tissue. We think this is closer to 3 weeks or 21 days or so.
In my practice, I extend that data to include Descovy, although there’s probably a difference between the two. But just for precautionary measures, we typically will also generally recommend the same amount of time, 7 and 21 days, with the rectal and vaginal tissue respectively.
For penile tissue, oropharyngeal tissue, or the throat, for example, we don’t have as good data, but largely, I would recommend closer to a 2 or 3-week mark in that regard. But the data that we do have rectal tissue 7 days vaginal tissue, approximately 21 days for injectable Apretude. We believe there is about a 7 to 14-day window before the drug achieves protective levels in the blood after your first injection.
So I often will inform my patients, who are already on some form of oral PrEP, to continue their oral PrEP for approximately 14 days after their 1st injection, to ensure that the injectable Apretude has reached levels that are protective against HIV.
Dr. Shuter: Dr. Bernardo, I want to follow that question up with a question about event-driven PrEP. And I suspect that some people on the call will be familiar with the idea or the concept of 211 dosing. We have to be careful about what we say here and really disclaim our statements and the content that’s going to follow by saying that this is not an FDA=approved indication of the medication as of yet, but it is something that is done very widely. It is approved by a number of very authoritative medical boards, and it might be coming, you know, in an official way, in the United States. So I suspect that people are doing it already. So what about you had just said that it takes, anyway, anywhere from a week to 3 weeks to build up a protective level when you use Truvada or Descovy the correct way. What about this 211 dosing? Tell us about that, and tell us how quickly protection is thought to kick in.
Dr. Bernardo: So 211 PrEP. Also known as on demand, PrEP, or event driven PrEP, is a way to reduce your pill burden – the number of pills you’re taking over the course of the month. This is particularly beneficial for individuals who are having sex with a perceived risk for HIV relatively infrequently throughout the month. It is currently recommended particularly for men who have sex with men.
The idea behind it is that you take and I will also mention that this is particular to Truvada, both the brand Truvada and generic Truvada. This is not currently recommended with Descovy. So again, Truvada generic, Truvada, 211 on demand or event-driven PrEP.
So the idea is you take two pills 2 to 24 hours before anticipated sex. So this is one of the downsides of this form of taking PrEP, because there is some anticipation that is required. So you take two pills, 2 to 24 hours before sex. Assuming you have sex during that time period, you take one pill 24 hours after the two pills, and then one pill 24 hours after that pill.
So two pills, 2 to 24 hours before sex, one pill 24 hours later, and then one more pill 24 hours after that.
The idea is that you are achieving protective levels within two hours after taking that loading dose of two pills. But it is important to follow with that 48 hour tail of medication. So one pill every 24 hours for 48 hours.
Here’s the caveat. If you were to have sex within that 48 hour tail, you have to take one pill every 24 hours for 48 hours after the last time you had sex. So you can imagine if you had sex two or three times in that week, you effectively are taking daily PrEP.
So again, this is a great idea for someone who has a perceived or actual risk for HIV, relatively, infrequently, for also for someone who’s looking to reduce or minimize their pill exposure.
Dr. Shuter: Dr. Felsen, I’m just going to present a couple of real world scenarios with regard to adherence and taking the medication properly. So I think we’ve tried to hammer home the idea that this medicine only works if you take it and take it as you’re supposed to. But what happens if my routine is to take it at 8 am every morning. And then one day at dinner time, I realized I didn’t take my 8 am dose. That’s scenario number one.
Scenario number 2 is, what if I miss a whole day? You know I missed my Thursday dose. And here’s Friday, and am I still protected? And what should I do? Should I double dose? Or what’s the correct approach, then?
Dr. Felsen: Yes, that’s a great question. And you can imagine that this comes up all the time, and nobody’s perfect, and nobody is going to be expected to take their medication at the exact same time every day 365 days a year. So this definitely comes up and we have to have real world expectations of our patients. And so the idea is, you want to do the very best that you can. So let’s say you take your pill. Let’s say you’re on Descovy or Truvada, and you take your pill every day at the same time at 8 am. And come that evening, you realize you haven’t taken it yet? Go ahead and take it, and you’re going to be just fine. You’re within the same 24 hours. It’s just fine, and you’ll be able to take your next pill at 8 am the next day without having to worry about it. That would be for the 1st situation that you said so like it it is. Let me just be very clear, it’s better to take it late than to skip it entirely. If you realize in the same day that you missed a dose, just take it later in the day, and you’ll be fine.
If you entirely missed a day, don’t double up on your meds. So if you missed your Monday dose, and now you wake up on Tuesday and said, Oh, my God! I forgot to take it. Take your Tuesday dose and forget about the Monday dose. It should be all right. Everyone is, you know, the idea is to take it as consistently as you can. We want to make sure that you take it almost every day. But if you miss a day. It’s not worth the potential risk of having too much medication on board by doubling up that day.
Dr. Shuter: We don’t encourage anyone to miss doses, but there are a great deal of data available to show that if you get six doses in a week rather than seven, that the protection should last throughout the week. So try to take every pill. But if you miss one dose, there’s nothing to panic about. And your protection probably continues.
Dr. Shuter: So, Dr. Bernardo, people’s circumstances change sometimes. So what if someone’s relationships change or they leave a relationship and aren’t in a new relationship, and their risk for HIV acquisition does, in fact, go to zero for a period of time. What is the story on whether you could start and stop PrEP. And if that is possible, then how do you go about doing it?
Dr. Bernardo: So obviously things, life, circumstances, change, relationships come and go, and so can PrEP. People can stop and start PrEP as they feel is necessary. However, we do recommend it is done under the guidance of a healthcare provider, for a couple of reasons.
In terms of discontinuing PrEP. Dr. Felsen had alluded earlier about checking for underlying hepatitis B infection prior to starting PrEP. The same is true when you stop PrEP. If it was missed initially and again, just to remind everyone, the reason is because these oral forms of PrEP do have activity against hepatitis B as well. And if an infection is missed, and these oral forms are stopped, you can actually have a rebound infection and can develop fulminant liver failure. And so we do have to screen. If it wasn’t screened for initially, if someone does have chronic hepatitis B, they do need to remain on at least one form of hepatitis B medication that that individual can discuss with their provider.
In terms of restarting PrEP, again, similarly, things change and people can definitely restart. However, prior to restarting PrEP, you do need an HIV test to make sure that you are, in fact, HIV-negative before restarting PrEP. So you should never just keep the pills at home, decide to stop for a month or two and then pick it up, you know, two, three months down the road without discussing with the healthcare provider, because those tests do need to be repeated, and to make sure we aren’t missing anything.
When it comes to the injectable form of Apretude, there is an additional concern. Apretude does have a very long what we refer to as a tail, meaning that after the injection it does take a while before the medication is completely eradicated from the body. And the reason this is concerned is because if someone does have an HIV exposure during this quote unquote tail period, they may still get infected, they may still get HIV. But now, because you have that low level drug available in your system, the HIV virus can become resistant to that medication, and not that we couldn’t treat the HIV infection. But we have to be a little bit more creative with our medications. So that’s an additional nuance in terms of starting and stopping PrEP when it comes to the injectable. Not that someone would do this at home, since it has to be done in the healthcare provider’s office, but something to keep in mind. If you do stop PrEP, or if you do stop injectable PrEP, if you feel that there may be a potential risk for HIV acquisition, make sure you’re using some other form of HIV prevention like condoms, for example, until you are able to return to your doctor’s office to discuss restarting injectable Apretude.
Dr. Felsen: And I would just add also that when you do restart, the same sort of timeframes that we’ve talked about earlier come into play again. So if you stopped PrEP, but now you’ve restarted again, it’s seven days before, if you’re on oral PrEP, it’s seven days before the protection in the rectal tissue, and about 3 weeks in the vaginal tissue.
Dr. Shuter: Thank you. So I I’d like to move on from the somewhat scientific discussion that we’ve had to maybe a bit of a philosophical view. And this is for Dr. Bernardo. We started off by talking about how patients might be embarrassed when they begin to approach this topic, and the topic is wrapped up in the idea of vulnerability that someone is vulnerable to being exposed to HIV and potentially acquiring HIV.
But those are kind of negative takes – embarrassment, vulnerability. Can you say a couple of words about how the decision to start PrEP can be empowering in an expression of a person’s power.
Dr. Bernardo: I like to refer to PrEP as a part of someone’s sexual health toolbox. Right? So when we talk about sexual health, there’s lots of different things we talk about. So we talk about contraception. We talk about vaccinations against certain sexually transmitted infections. Sure, we talk about condom use. We talk about PrEP, we talk about family planning. There’s a lot that goes on there, and I feel that PrEP and HIV risk is just a small part of that.
So whenever I have conversations regarding sexual health with my patients, I’m not just focusing in on that one thing. I’m not. Because then what happens is you’re equating sex and HIV. It becomes this direct link, this direct association, when sex is more than just about your risk for HIV. It’s a small part of it. And so I make that conversation part of a larger conversation, and again, by normalizing the conversation to your point earlier. Anyone who’s having I forgot how exactly how you phrased it. Non zero percent risk.
These conversations should be brought to the table. So by normalizing the conversations around PrEP. And I ask it. I usually ask it in a very sort of non-discriminating, non-offensive way. I say, so tell me what you’re doing to keep yourself that you’re enjoying sex you’re doing in a way that’s keeping you safe. Talk to me about the tools you’re using for prevention against sexually transmitted infections. Right? And I might not even mention HIV right away. And sometimes condoms come up. Sometimes patients will say, Well, I try to use condoms as often as I can, but sometimes I forget, and then I’ll use that as an opportunity and say, Well, have you heard about HIV? Pre-exposure prophylaxis? And sometimes that’s a way to sort of drive the conversation. But to get back to your original question. I think the big point to be made here is that we have to get away from associating sex and HIV, that it’s more than just that. It’s not just about HIV prevention when we’re having these conversations, both on the side of the healthcare provider and the side of the patient. These are part of much larger conversations as we normalize conversations around sexual health. So that’s that’s one way that I try to strategize.
I bring these conversations to the table, and patients should not feel uncomfortable having these conversations, because, like I said earlier, many, many people want to have these conversations. They just don’t know how to have them. So let’s normalize the conversation. Let’s talk about it.
Dr. Shuter: Thank you. And you know. So both my patients and my colleagues know that I’m something of a zealot about general health care. And I also want to make the point, and I think what Dr. Bernardo just said is a good segue into it, that we want to normalize sexual health, but that implies that it becomes part of your overall health care. And for anyone out there who is contemplating looking into PrEP and contacting a provider, it would be a tremendous missed opportunity to not pull other health issues into that conversation. Because, yes, this is important. But if you smoke cigarettes, that’s really important also. And if you have hypertension, that’s really important, and if your lipids aren’t good, or if you’re diabetic, or you’re suffering with obesity, or you’re struggling with depression or anxiety. These are all major major medical issues, and they are all very common.
And to me it would be something of a tragic error to interact in an intensive way with the medical community and to leave that stuff out. Now, the truth is that your PrEP provider may very well not have time in the visit that’s allocated to you to deal with those things.
But at the very least they should enter the conversation because he or she might feel comfortable dealing with them at future visits, or might feel comfortable referring you to a different provider. Because if you’re going to get this part of your health in order, go ahead and get all the parts of your health in order, it’s a great opportunity to do that, and a great way of getting started and being healthy from A to Z. So I do want to make that point.
Dr. Shuter: At this point I would like to invite Dr. Felsen and Dr. Bernardo to contribute any final thoughts. Is there anything we left out anything niggling at you that we ought to say.
Dr. Bernardo: I I guess the one thing I will add is to remember and forgive me for being repetitive, but I think it’s important that talking about sexual health isn’t just about HIV prevention, and I think it’s important to have conversations about other ways to improve your sexual health toolbox, and these are things like, for example, talking about contraception. If you’re capable of getting pregnant, talk about vaccinations that are available against certain sexually transmitted infections, like, for example, hepatitis B, or the human papillomavirus.
So these lead to sort of broader conversations, and if your healthcare provider doesn’t bring it up, I encourage you as patients to bring those things, those topics to the table as well.
Dr. Felsen: I think that’s a that’s a great point. I I just want to add that PrEP is a really important tool of that toolbox. And right now it’s being underutilized. Not enough people who would benefit from it are using it. And so we need to keep thinking of ways to make sure that those who have the most to benefit from this advance can get their hands on it. And can, you know benefit from its effectiveness.
Dr. Shuter: Thank you, and I would like to circle back also to adherence, because, as I said at the beginning, that is really the Achilles heel of the pills that patients take. So it is adherence, adherence, adherence, and we are talking to an audience of smart people.
We can’t understand and advise you about every circumstance in your life, so I don’t know what adherence strategies are going to work for you. It might be putting your pill next to your toothbrush every day.
It might be putting it next to the coffee maker, as a reminder to take it every day. But you have to also anticipate other situations. What are you going to do when you go on vacation? The time to think about it is not when you’re running to the gate in the airport. The time to think about that is the day before. What should I do? Where should I pack this?
Or, if you’re going to go sleep at a friend’s house for the night, and be out of your house for 24 hours. How can you take the pill along in a way that works for you, because if you don’t think of those things in advance, they’re not going to happen, and your adherence is going to fall down, and when PrEP fails, it is because patients don’t take their pills. Right? So please give that some thought. If you’re contemplating starting PrEP, or you’re on it now, think about how to stay on it really, really, reliably, over the course of time.
Moderator: Thank you very much, Dr. Bernardo, Dr. Felsen, Dr. Shooter, for participating tonight. And thank you to our audience for joining us.
If you want more information, you can visit our PrEP for Patients Resource Center at pcmedproject.com, where there’s written material, podcasts, and infographics.
The CDC also has excellent materials for consumers at CDC.gov. They call it “Let’s Stop HIV together.”
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose

Cervical Cancer Screening and Management: Challenging Cases
Review the latest recommendations with
Emma L. Grabinski, MD, FACOG
Dr Grabinski, a generalist OBGYN, is System Chief of OBGYN & Perinatology at Swedish Medical Center, and a clinical adjunct Professor at UW in Seattle WA
Learning Objectives: Upon completion of this activity, participant should be better able to
- Discuss cervical screening and management of immunocompromised people
- Describe cervical screening and management post treatment for malignancy
- Counsel patients in unusual screening and management situations, applying knowledge of hrHPV biology
SUMMARY:
The new ASCCP management guidelines provide recommendations on the management of cervical cancer screening abnormalities. But sometimes, we have to deal with unusual or more challenging situations. The key point to remember with the following, less typical clinical scenarios is that successful outcomes hinge on not only following best practices but individualizing care.
CONTENTS:
- Case 1: Immunocompromise
- Case 2: Limited Prior Screening
- Case 3: Persistent hrHPV
- Case 4: Testing after History of Malignancy or CIN 2/3
- Case 5: Post Coital Bleeding
Case 1: Immunocompromise
17 year old recently became sexually active, wants to discuss contraception options. She has a history of Crohn’s disease that is well controlled with a biologic. You suggest cervical cancer screening, but the patient is surprised – she thought Pap screening didn’t start until age 21
- Immunocompromise, due to HIV and non-HIV related causes
- Increases the risk for hrHPV-related cervical dysplasia and malignancy
- Requires more intense screening, surveillance, and treatment
Who to Screen
- HIV infection
- Solid organ transplant recipients
- Hematopoietic stem cell transplant recipients
- IBD on immunosuppressants
- SLE – regardless of treatment
- RA on immunosuppressants
How to screen
- Starting age
- 21 years or within 1 year of sex if immunosuppressed <21 years
- Screening strategy
- <30 years: Cytology preferred
- ≥30 years: Co-testing preferred | Cytology acceptable
- Repeat every 1 to 3 years
- Recent data of HIV infected people suggests that after a period of intense screening, the interval can be lengthened
- When to stop
- Continue past age 65 | Discontinue screening based on shared discussion regarding quality and duration of life rather than age
How to Manage
- Neg Pap/hrHPV+ or ASCUS with unknown or hrHPV-
- Repeat in 6 to 12 months
- ASCUS or hrHPV+
- Colposcopy
- ASCUS or higher-grade lesion and hrHPV+
- Colposcopy
- Risk of immediate CIN 3+ is always >4% in the immunocompromised population
Case 2: Limited prior screening
32 year old new patient presents for pelvic pain discussion. They deny previous abnormal Pap results, but you do not have records. They are unsure when they last had a Pap. Current screening results show ASCUS and hrHPV+
- Risk of immediate CIN 3+ is >4% (based on cytology results)
- Recommendation is for colposcopy
- Rarely screened patients are at higher risk
- We are not able to be certain whether hrHPV+ result represents a new infection or persistence
- Race, ethnicity, and socioeconomic considerations all contribute to lower screening rates for cervical cancer
- Discrepancies in access to follow up results in higher rates of cervical cancer
- Opportunistic screening is important in the following clinical settings
- Limited prior screening
- Reliability for follow up is reduced (often related to social factors, including limited access to healthcare resources)
Case 3: Persistent hrHPV
52 year old established patient, presents for colposcopy due to a report that is negative for intra-epithelial lesions and malignancy (NILM) and hrHPV+. This is their 4th consecutive colposcopy for the same result. Current and previous colposcopy does not show CIN 2/3+. She is frustrated and wonder if they need to continue doing colposcopy
- HPV persistence is essential for development of cervical cancer
- Current ASCCP/ACOG guidelines recommend repeat co-testing in 1 year, with colposcopy if ASCUS+/hrHPV+
- The Swedescreen Study showed that HPV persistence (with normal colposcopy) over 6 years resulted in either high rates of CIN2+ or clearance
- No cases of invasive cancer were identified in this 6 year interval
- However, continued annual testing may result in non-attendance for follow up
- Loss to follow-up may potentially result in failure to identify people with CIN 2+
- Evidence of HPV persistence after treatment for CIN shows that there is significant clearance of HPV within 24 months after LEEP or conization
Counseling Options for This Patient
- Continued screening
- ASCCP approved interval: Annually until either clearance of HPV or development of CIN 2+
- May extend screening interval that is acceptable to patient | Should be demonstrated that patient will be reliable with follow up
- Treatment
- HPV clearance has been demonstrated after LEEP or conization: May be reasonable option for patients wishing to avoid long term follow up
- Hysterectomy is not recommended for treatment of hrHPV | However, in people with no desire for future fertility and who may have other indications for hysterectomy, this approach may be a reasonable option
Case 4: Testing after Malignancy or CIN 2/3
A 47 year old patient presents 5 years after radical hysterectomy for Stage 1(b)i squamous cell carcinoma of the cervix. They have ‘graduated’ from follow up with gyn oncology and are here for a preventive exam. They wonder whether they should still have pap smears.
Hysterectomy for CIN 2/3
- Primary vaginal cancer extremely rare – however is significantly higher in this population.
- 0.4-0.6/100,000
- hrHPV+ prevalence of the vagina is similar whether hysterectomy has, or has not been done
- Hysterectomy for CIN2/3 will NOT result in clearance of hrHPV
- Accuracy of vaginal cytology and hrHPV testing has not been determined for diagnosing VAIN2/3
- PPV ranges from 0-14%
- Per ASCCP, patients should be followed with cytology every 3 years for a minimum of 25 years after hysterectomy
- Depends on life expectancy and degree of co-morbid conditions
- Discuss whether patient would have further intervention for VAIN 2/3 or malignancy to determine whether to screen or when to stop screening
- Risk after hysterectomy for CIN 2/3 similar to risk of vaginal cancer after treatment for invasive cervical cancer
- Consider not performing after counseling based on low risk of developing malignancy
- Colposcopy recommended for the following
Endometrial Cancer
- Most recurrences happen at the vaginal cuff
- Cytology has been shown to be abnormal in 25% of recurrence
- However, most recurrence is detected based on clinical symptoms
- Abnormal cytology may also represent radiation changes
- Cytology has not been shown to add clinical benefit and is not recommended
Ovarian Cancer
- Cytology not recommended
Cervical Cancer
- 75% of recurrence occurs in first 3 years
- NCCN recommends follow up every 3 to 6 months in first 2 years, and then every 6 months for the next 3 years
- Most will present with symptoms (46 to 95%)
- Physical exam detects asymptomatic recurrence in 29 to 75% of people
- Abnormal cytology
- Rarely the only abnormal finding
- Does not significantly increase detection rates | Only up to 17% of cases will be based on cytology alone
- The rate of abnormal cytology in people with prior radiation and no recurrence can be up to 36% | Most are ASCUS
- SGO ‘Choosing Wisely Campaign’ recommends
- Vaginal cytology (if used) no more frequently than annually
- No colposcopy if cytology shows less than high grade changes
Vulvar/Vaginal Cancer
- Usually HPV mediated
- Cytology
- Not recommended for follow-up to detect recurrence | Reserved cytology for HPV related cervical premalignant disease
- Should have annual comprehensive vulvar exam to detect recurrence
Case 5: Post Coital Bleeding (PCB)
44 year old presents with a 6 month history of abnormal bleeding. On evaluation, the bleeding is occurring mainly after penetrative intercourse. She reports her last Pap was 3 years ago and was normal
- Cervical cancer screening guidelines (ASCCP, ACS, USPSTF) are for ASYMPTOMATIC patients only
- Patients with abnormal bleeding do not fit into these algorithms, and visualization of the cervix with sampling of the cervix with cytology and/or biopsy may be appropriate
- Send these results for ‘diagnostic’ NOT ‘screening’ interpretation
- Prevalence of cervical cancer is 3 to 5.5% in people with PCB
- PCB is the presenting complaint in 11% of people with cervical cancer
Cervical cancer is very unlikely in the following situations and therefore colposcopy may not be clinically appropriate if pelvic exam benign
- <21 yo
- Regardless of age:
- Negative cytology in the past 12 months
- Negative co-testing in the past 3 years
Consider colposcopy if the following applies, regardless of screening results
- Visible cervical lesion
- Persistent PCB
- PCB with persistent minor cytological anomalies
- Immunocompromised
- at risk for inadequate cytological screening
- Other causes to consider when assessing a patient with PCB
- Polyps | Infection | Atrophy | Other genital tract malignancy (vaginal or endometrial cancer) | Sexual abuse
REFERENCES:
Commercial Support
This educational activity is supported by Hologic
Faculty Disclosures
Dr. Grabinski reports that she has no relevant financial relationships to disclose

Cervical Cancer Screening Guidelines – Key Points for Shared Decision Making with Your Patients
Review the latest recommendations with
Emma L. Grabinski, MD, FACOG
Dr Grabinski, a generalist OBGYN, is System Chief of OBGYN & Perinatology at Swedish Medical Center, and a clinical adjunct Professor at UW in Seattle WA
Learning Objectives: Upon completion of this activity, participants should be better able to
- Apply current evidence regarding cytology and HPV detection when counseling patients about cervical cancer screening options
- Discuss the natural history of HPV infection and the impact of the virus in determining the risk of cervical dysplasia
- Describe the current screening recommendations for immunocompetent people
CONTENTS:
- Case
- Synopsis
- Professional Guidelines and Key Points for Shared Decision Making
- The Wrap-Up
- References
THE CASE:
- 36-year-old G1P1
- Presents for preventive exam | Otherwise well
Gyn History
- No significant gyn issues in past 10 years
- Pap smears (cervical cytology) every 3 years since age 21
- Monogamous | Received full HPV quadrivalent vaccine dose
- Previous cervical cancer screening results (3 yrs prior)
- Negative for intraepithelial lesion or malignancy (NILM) | Negative for high risk HPV (hrHPV)
- Patient has read there are new guidelines for screening and would like to discuss options, including continued co-testing, cytology alone, or HPV testing alone
SYNOPSIS:
Cervical Cancer Overview
- Cervix cancer is more common than vulva, vaginal, or penile cancer as HPV infects the transformation zone of the cervix, which is immature, metaplastic and hormonally responsive (McMurray et al. Int J Exp Pathol, 2001)
- HPV’s ability to infect immature tissue is thought to contribute to the higher likelihood of premalignant, and malignant transformation
- In contrast, the remainder of the genital tract is mature epithelium
- HPV Infectivity
- Most people will be become infected with HPV soon after first intercourse
- Most of these infections will clear
- 67% clear within first 12 months (Rodríguez et al. J Natl Cancer Inst, 2008)
- Long duration of infectivity predicts the risk of progression to pre-malignant and malignant transformation (Schiffman and Castle. NEJM 2005)
- Takes time for mutations to accumulate and for the cells to become immortal
- Mean age of diagnosis of cervical cancer (Wheeler et al. J Natl Cancer Inst, 2009)
- HPV 16: 48.1 years
- HPV 18: 45.9 years
- Other high-risk HPV types: 52.3 years
Professional Guidelines Options and Shared Decision Making for Women (30 to 65 years)
ACOG, ASCCP and SGO have endorsed the USPSTF cervical cancer screening recommendations
Co-testing (cervical cytology and hrHPV testing) every 5 years
- Pros
- Co-testing with cytology and hrHPV testing is more sensitive than cytology alone
- Identifies people at higher risk of developing precancerous lesions
- In women >30 years, liquid-based cytology/HPV cotesting improved screening for cervical cancer vs liquid-based cytology or HPV components alone (Kaufman et al. AJCP, 2020)
- Although not designed for this purpose, abnormal glandular lesions may be detected, possibly representing endometrial pathology
- Determines those who need shorter screening intervals
- Cons
- More costly than hrHPV testing alone or cytology alone
- Patient anxiety with prolonged screening intervals
Screening with cervical cytology alone every 3 years
- Pros
- High specificity when abnormal (Kudva. AJCP, 2015)
- Avoids detecting transient hrHPV infection
- May reduce psychological harm associated with being labelled as having an STI
- Cons
- Fewer cases of precancerous lesions detected
- Cytology is less sensitive than HPV testing with regards to detecting precancerous lesions (Perkins et al. J Low Genit Tract Dis, 2020)
- Cytology has a false negative rate of 10-20% | False positive rate of 10-20% (Kudva. AJCP, 2015)
- Adenocarcinoma is not well identified on cytology
- Fewer cases of precancerous lesions detected
HrHPV testing alone as an alternative screening strategy (re-screen not more frequently than every 3 years)
- Pros
- Fewer unnecessary diagnostic tests – as hrHPV testing has
- Higher sensitivity than cytology alone, especially in vaccinated populations
- Fewer unnecessary diagnostic tests – as hrHPV testing has
- Cons
- HPV testing has a false negative rate of up to 5%
- An insufficient pap can clue the provider that the HPV result may be falsely negative
- Has a lower specificity than co-testing (Kudva. AJCP, 2015)
- HPV infection common
- However, persistence less common
- HPV alone may result in more diagnostic testing for lesions that would have regressed (Kaufman et al. AJCP, 2020)
- Requires use of an FDA approved hrHPV testing platform
- This is not available in all settings and requires the clinician to know what platform the lab uses
- If not an appropriate platform, can result in inadequate screening for the patient
- Management of positive hrHPV recommendations require reflex cytology on the same sample
- Delay in obtaining results may increase anxiety for patient
- HPV testing has a false negative rate of up to 5%
American Cancer Society (ACS)
Recommended for women 25 to 65 years of age
- HPV testing every 5 years
- Aside from risks related to higher false negative rates based ‘HPV only’ strategy (see above), there are also other concerns regarding the ACS strategy of HPV only spaced 5 years apart
- Management and follow-up: ACS recommendations differ in that there is no reflex cytology if abnormal hrHPV
Other Issues With ACS Recommendations
- Race, ethnicity and socioeconomic factors (Curry et al. JAMA, 2018)
- African American population: Receive screening at the same rate as white populations but 2x the rate of death from cervical cancer | Likely due to discrepancies in follow up and diagnosis
- Native/Indigenous populations, Hispanic populations, and Asian populations: Have lower screening rates than white populations
- White populations in poorer, rural areas are also disproportionally affected by cervical cancer
- Appropriate patient profile for ACS requires the following
- Patient is average risk given history of normal screening
- NO risk factors for immunocompromise
- Has demonstrated compliance with screening and follow up
- HPV vaccination rates in the USA are not high enough currently to factor vaccination into screening guidelines
The ACOG Practice Advisory
- The ACOG Practice Advisory Update recommends individualizing care, providing counseling, and allowing patients to choose the option that best suits them
The specific strategy selected is less important than consistent adherence to routine screening guidelines. Inadequate cervical cancer screening remains a significant problem in the United States, with persistent health inequities across the entire spectrum of cervical cancer care
The Wrap-Up
Patients Are Individuals and Deserve Individualized Care
- Screening for asymptomatic individuals currently include the following options
- Cytology with co-testing | Cytology alone | HPV with or without reflex cytology
- HPV 16/18 have the highest risk for development of CIN 3+ – do genotyping whenever possible!
- Cytology is not effective at detecting adenocarcinoma
- The most effective way of preventing cervical adenocarcinoma is with HPV vaccination
- Cytology is important for individualizing the follow-up interval (see ASCCP risk-based guidelines in ‘References’ below)
- Patient should be aware that even in the setting of HPV only strategy, an HPV positive report will default to ASCCP recommended follow up, which includes cytology
- New recommendations that favor HPV testing alone do not account for
- US HPV vaccination rates
- Lack of universal health care
- Race and ethnicity related differences in cancer rates and access to care
- Educate your patients that
- A preventive visit does NOT equal a pap smear
- Not needing a pap smear does NOT mean you don’t need a preventive visit
REFERENCES:
Biology of human papillomaviruses (McMurray et al. Int J Exp Pathol, 2001)
The Promise of Global Cervical-Cancer Prevention (Schiffman and Castle. NEJM 2005)
ACOG Practice Advisory: Updated Cervical Cancer Screening Guidelines
Commercial Support
This educational activity is supported by Hologic
Faculty Disclosures
Dr. Grabinski reports that she has no relevant financial relationships to disclose

The Evidence Behind Testing Strategies for Cervical Cancer Screening – Implications for Your Practice
Review the latest recommendations with
Sarah M. Temkin, MD, FACOG
Dr. Temkin is a gynecologic oncologist and equity advocate
Learning Objectives: Upon completion of this activity, participants should be better able to
- Understand the benefits and the risks of cervical cancer screening
- Become familiar with the clinical trials that led to the evidence for current cervical cancer screening guidelines and recommendations
- Compare the efficacy of different screening options, cytology, contesting, primary HPV testing for different age groups
- Consider the best frequency and type of screening for an individual patient and your practice population
CONTENTS:
Currently, women ages 30 to 65 have multiple options when it comes to cervical cancer screening. These options include (1) co-testing (cervical cytology and HPV testing), (2) cervical cytology only and (3) HPV only. How clear is the evidence behind these options?
BACKGROUND:
- Cervical cancer remains a major public health concern
- Globally: > 500,000 women per year affected | Fourth most common cause of cancer death among women worldwide (Arbyn et al. Lancet Global Health, 2020)
- US: Estimated 13,800 women will be diagnosed with cervical cancer in 2020 and more than 4,000 of women will die(Siegal et al. A Cancer Journal for Clinicians, 2020)
- Human papillomavirus (HPV) causes most cervical cancers
- ≥70 percent of cervical cancer cases attributed to HPV-16 and HPV-18 | The remainder are caused by other high-risk HPV types (Munoz et al. NEJM, 2003)
- Sexual transmission is a nearly exclusive pathway of HPV transmission | HPV estimated to be most common sexually transmitted infection in the US | By age 50 approximately 80% of women have been infected with some type of HPV (Nielsen et al. Sexually Transmitted Diseases, 2008)
- Most women who acquire the HPV virus do not develop cervical cancer
- 90% of HPV infections resolve on their own within 2 years | A small number of women do not clear the HPV virus and are considered to have a persistent infection (Munoz et al. NEJM, 2003)
- Cervical cancer is a preventable malignancy and worldwide eradication is a feasible goal
Cervical Cancer: New Cases, Deaths and 5-Year Relative Survival (credit SEER)
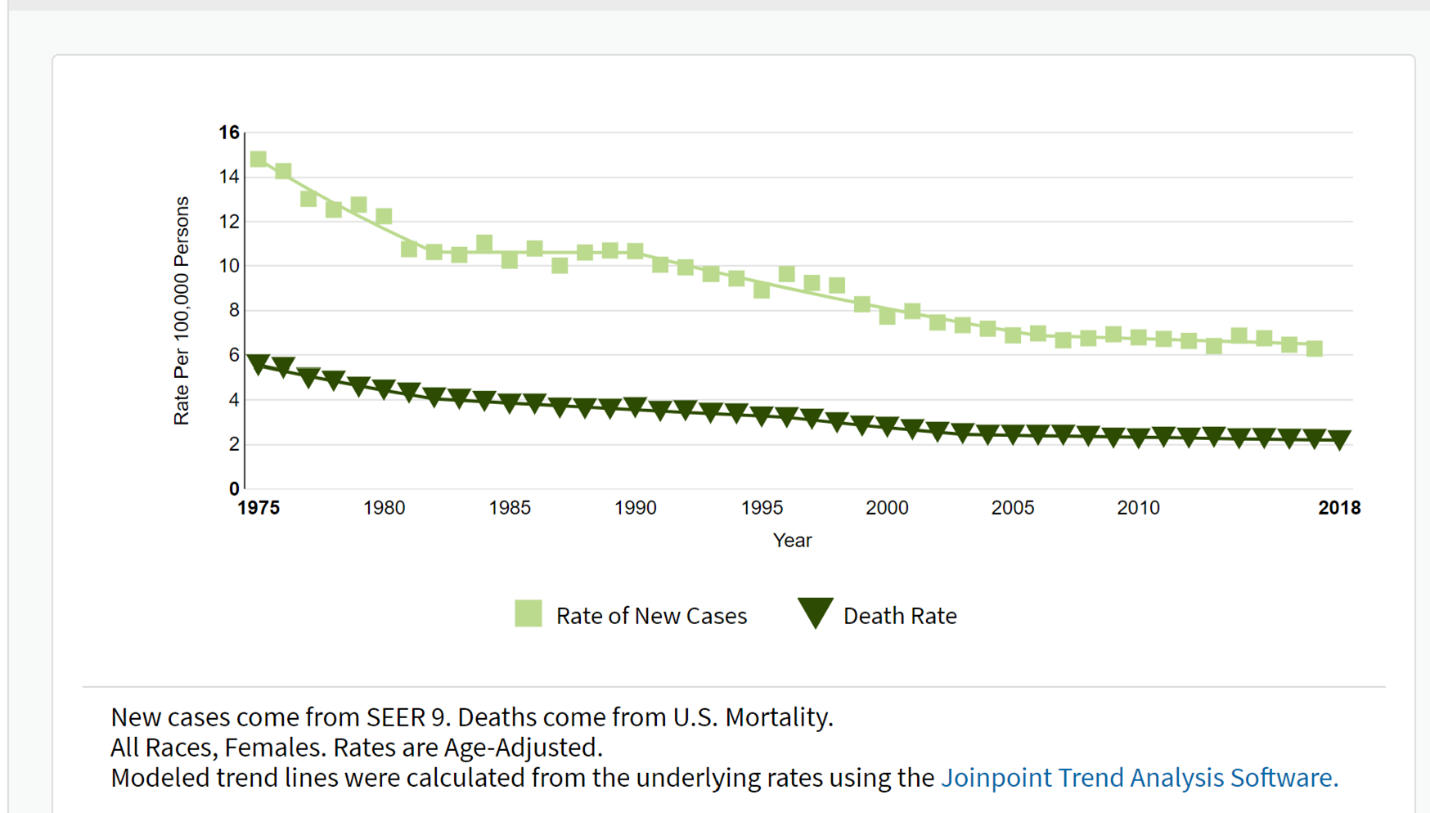
Note: Most women who have abnormal cervical cell changes that progress to cervical cancer have never had a Pap test or have not had one in the previous three to five years
KEY CONCEPTS WHEN IT COMES TO SCREENING:
What are the Harms of Overscreening?
- Tumor biology drives the efficacy of screening for an individual disease (Esserman et al. Lancet Oncology, 2014)
- For very slow growing conditions or precancerous lesions that may regress without treatment such as cervical cancer, screening too frequently may lead to overdiagnosis – the diagnosis of a condition that would not have required treatment if it had not been diagnosed
- Screening has downstream consequences
- Cost | Time away from work and other activities | Occasional physical discomfort
- False positive screening results can lead to unnecessary follow-up tests (e.g., invasive biopsies, anxiety)
- Colposcopies, LEEPs and cone biopsies are uncomfortable
- Excisional biopsies in nulliparous patients may increase the risk of preterm delivery
Overdiagnosis: Size vs Time (credit NCI)

What are the Benefits Related to Cervical Cancer Screening?
- Cervical cancer is a preventable malignancy and worldwide eradication is a feasible goal
- Screening can alter the natural history
- Screening allows for detection and removal of high-grade precancer
- Allows for the early detection of invasive cervical cancer
- Widespread adoption of pap smear screening in the US during the 1950’s and 60’s led to significant declines in incidence and mortality
- Overall incidence rates for invasive cervical cancer decreased by 54% over the 35 years from 1973 to 2007
- Most women who have abnormal cervical cell changes that progress to cervical cancer have never had a Pap test or have not had one in the previous three to five years
KEY PUBLICATIONS:
HPV vs Cytology
Ronco et al. Lancet, 2014
- Combined results of 4 randomized trials in Europe (Sweden, Netherlands, England and Italy)
- Participants
- Women ages 20 to 64
- Study design
- Different protocols between studies
- Randomized to HPV-based or cytology-based screening
- Results
- 176,464 participants
- HPV-based screening provides 60-70% greater protection against invasive cervical carcinomas vs cytology
- Rate ratio of 0.60 (95% CI, 0.04-0.89) in favor of HPV testing for the detection of invasive carcinoma
Leinonen et al. BMJ, 2012
- Prospective randomized trial in Finland
- Participants
- Women ages 25 to 65
- Study design
- Participants followed over one screening round of five years
- HPV group (followed by cytology if positive): 101,678 women
- Primary cytology group: 101,747 women
- Participants followed over one screening round of five years
- Results
- Hazard ratio: 1.36 (95% CI, 1.09-1.59) for detection of CIN3/AIS for primary HPV screening
- Cumulative detection rate was 0.0057 (0.0045 to 0.0072) for HPV screening vs 0.0046 (0.0035 to 0.0059) for conventional screening
- “HPV screening could increase the overall detection rate of cervical precancerous lesions only slightly”
Ogilvie et al. JAMA, 2018
- Prospective randomized clinical trial in Canada
- Participants
- Women ages 25 to 65
- Study design
- Participants followed for (CIN) grade 3 or CIN3+ detected up to and including 48 months
- HPV group: 9552 women | Negative status returned in 48 months | Reflex cytology for positive HPV results
- Cytology group: 9457 women | Negative status returned in 24 months | If negative at 24 months, returned at 48 months | Followed by reflex HPV testing for women with ASCUS
- Participants followed for (CIN) grade 3 or CIN3+ detected up to and including 48 months
- Results
- The CIN3+ incidence rate (primary outcome)
- HPV group: 2.3/1000 (95% CI, 1.5-3.5)
- Cytology group: 5.5/1000 (95% CI, 4.2-7.2)
- CIN3+ risk ratio: 0.42 (95% CI, 0.25-0.69)
- For patients who were negative at baseline
- HPV-negative women, had a significantly lower cumulative incidence of CIN3+ at 48 months than cytology-negative women | CIN3+ risk ratio, 0.25 (95% CI, 0.13-0.48)
- “…by adding cytology to the intervention group, an additional 3 CIN2+ lesions were detected in HPV-negative women. In contrast, by adding HPV testing to the control group, HPV testing detected 25 CIN2+ lesions that would not have been detected by cytology alone”
- The CIN3+ incidence rate (primary outcome)
Sankaranarayanan et al. NEJM, 2009
- Prospective randomized trial in rural India
- Participants
- Women ages 30 to 59
- Low resource setting
- Randomized to 4 groups
- HPV group
- Cytology group
- Visual inspection with acetic acid (VIA) group
- No screening (standard of care)
- Results
- There was a decrease in cervical cancer deaths among the HPV group vs standard care (no screening)
- Hazard ratio 0.52 (95% CI, 0.33 to 0.83)
- Reduction is deaths driven by ‘stage migration’ (a lower stage at diagnosis for women who developed cervical cancer)
- Cytologic screening or VIA did not lower the cervical cancer mortality rate
- There was a decrease in cervical cancer deaths among the HPV group vs standard care (no screening)
Relative Contributions of Cytology and HPV tests within Cotesting
Kaufman et al. AJCP, 2020
- There are no head-to-head studies that evaluate co-testing vs HPV only
- Kaufman et al. performed a review on a large commercial database (2010 to 2018)
- 13,633,071 women ≥30 years | Diverse population in the US
- 18,832,014 cotest results
- Goal of the study: To evaluate the results of liquid-based cytology and HPV testing in cotesting preceding cervical cancer and precancer diagnoses
- Results
- 1,615 cotests preceded 1,259 cervical cancer diagnoses | 11,164 cotests preceded 8,048 cervical precancer diagnoses
- More women subsequently diagnosed with cervical cancer within 1 year of cotesting were identified by cytology result (P<.0001)
- Cytology: 85.1%
- HPV: 77.5%
- More women subsequently diagnosed with CIN3/AIS within 1 year of cotesting were identified by HPV result (P<.0001)
- Cytology: 89.3%
- HPV: 97.6% was more frequently positive than LBC prior
- False-negative rate in women with cervical cancer
- Positive cytology/negative HPV: 13.1%
- Rate increases if testing >12 months
- The authors conclude
…Liquid-based cytology (LBC)/human papillomavirus (HPV) cotesting enhances screening for detection of cervical cancer in women 30 years an older, more so than LBC or HPV alone among women receiving cotesting
…detection of prevalent “precancers” (detection sensitivity) is likely to overestimate the effectiveness of any screening formulation in preventing invasive cancer
Because of this bias, the performance of screening tests targeting the diagnosis of invasive cancer as the primary end point of screening effectiveness is especially relevant
THE WRAP UP:
Evaluating the Studies
- HPV‐based cervical cancer screening has superior sensitivity and long‐term negative predictive value compared with cytology‐alone screening demonstrated in several randomized controlled trials
- However, there are no direct randomized head-to-head studies between HPV only vs co-testing
- Large retrospective database studies of a heterogeneous population that compared HPV to co-testing suggest that HPV only may be better at detecting precancerous lesions but including cytology leads to better detection of cancers within the subsequent year
- Data from randomized controlled trials that assessed HPV only strategies may not be representative of the US population
- Adherence to follow-up in the real world may be quite different
- Few participants from under-represented minority populations with higher disease burden (Black and Hispanic participants in particular) were included in these trials
- Model‐based studies create a composite of epidemiologic, clinical, and resource data from various empirical studies and databases, yet uncertainties in the data and model structures are unavoidable
- Areas of remaining uncertainty include the following
- The effect of persistent HPV infection and reactivation
- Clinical course after acquisition of new infections at older ages | Increasing life expectancies and potential cohort effects because of changes in lifetime sexual behaviors of US women over time are unknown
When to Consider More Frequent Testing
- The new ACS guidelines recommend HPV only testing every 5 years, however, these guidelines assume this patient is not immunocompromised or is not at otherwise medically higher risk for persistent HPV infection
- Patients who are at higher risk and should be screened more frequently
- Immunocompromised: HIV | History of solid organ or stem cell transplant | DES exposure | Other conditions associated with decreased immune response
- Medical history: Previous CIN2, CIN3, or AIS | Extend screening past age 65
- Are there factors that may lead to patient being less likely to adhere to screening at a date later than when she is in the office?
- Social factors
- Health insurance insecurity
- Transportation barriers
- Trauma with pelvic examinations
- Is this patient symptomatic?
- Postcoital bleeding is a typical early sign of cervical cancer | A mass on the cervix requires a biopsy
- Interval cervical cancer screening may be indicated for patients with persistent vaginal discharge, pain, etc.
- Does this patient have a new partner? Does her partner have a new partner?
- This may especially impact discontinuation of screening in older patients
Disparities
- Disparities have decreased but continue to exist in incidence and mortality from cervical cancer based upon geographic location, rural/urban residence and for racial/ethnic minorities (Fleming et al. PLoS One, 2014; Temkin et al. Gynecologic Oncology, 2018)
- The contributors to these inequities include barriers such as access to follow-up and treatment
- Provider bias contribute to inequities | Be an upstander and find ways to help patients overcome structural inequities that may impact care (Temkin et al. Gynecologic Oncology, 2018)
Cervical Cancer Screening for Women <30 years
- While ACOG/ASSCP/UPSTF recommend starting screening at age 21, ACS recommends beginning screening at age 25
- Substantially higher HPV positivity rates have been demonstrated leading to higher colposcopy rates than with cytology alone or co-testing (Ronco et al. Lancet, 2014)
- In the prospective US screening study evaluating the performance of primary HPV screening in women aged ≥25 years, however, HPV testing was significantly more sensitive for the detection of CIN3+ than cytology alone (Wright et al. Gynecologic Oncology, 2015)
- Both HPV16/HPV18 positivity and cytologic abnormalities were highest in women aged 25 to 29 years, and more than one‐half of the women in this age group who had CIN2+ (or CIN3+) identified on colposcopy had a negative cytology result
- In light of the increased detection of abnormalities in this age group, adherence to conservative management guidelines is recommended
Cervical Cancer Screening for Women >65 years
- The evidence from randomized trials for screening after age 65 is limited
- Most trials included women up to age 65, not older
- Limited data for screening older patients who have a new partner
- Guidelines generally recommend to stop screening average-risk women >65 for cervical cancer no history of cervical intraepithelial neoplasia grade 2/3 or cancer and documented adequate negative prior screening
- However, because approximately 20% of new cases of cervical cancer are diagnosed in women ≥65 years of age, attention to patients in whom screening should continue is extremely important and include the following
- Patient without adequate prior negative screening defined as 2 consecutive negative HPV tests, or 2 consecutive negative co-tests, or 3 consecutive negative cytology tests within the past 10 years | Underscreening is common among patients over age 50 as the need for gynecologic care is often decreased
- Patients who are currently under surveillance for abnormal screening results
- Patients who are immunosuppressed
- Cervical cancer screening may be discontinued in individuals of any age with limited life expectancy
Vaccination
- Best public health strategy remains prevention associated with a substantially reduced risk of invasive cervical cancer at the population level
- HPV vaccine has been available since 2006 (Schiller et al. Vaccine, 2012)
- Vaccines if administered prior to the acquisition of HPV infection are highly effective at cancer prevention
- Wide variation across the US, with only about 50 percent of adolescents ages 13 to 17 up to date with the recommended regimen (Elam-Evans et al. MMWR Morb Mortal Wkly Rep, 2020)
- Vaccination rates in your community may impact population prevalence of HPV infection which will change the positive and negative predictive value of cytology or HPV testing
- Recent attenuation of declines in incidence, an increase in diagnoses of metastatic disease and growing percentages of adenocarcinomas underscore the importance of continued efforts to further reduce the burden of cervical cancer in the U.S (Islami et al. Preventative Medicine, 2019)
REFERENCES:
Cancer statistics, 2020 (Siegal et al. A Cancer Journal for Clinicians, 2020)
Screening for Cervical Cancer in Rural India (Sankaranarayanan et al. NEJM, 2009)
Commercial Support
This educational activity is supported by Hologic
Faculty Disclosures
Dr. Temkin reports that she is an advisor for Tesaro/GSK and Clovis for which she has received honoraria
Related ObG Project Topics
Screening for Cervical Cancer in the Woman at Average Risk

Sexual History Taking 101: How Do I Start the Conversation with My Patients?
Review the latest recommendations with
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Learning Objectives:
- Define sexual health and how it is applied in clinical settings
- Detail the burden of sexually transmitted infections (STI) in the United States
- Describe standardized guidelines to sexual history-taking
- Identify affirming approaches to successful sexual history-taking
CONTENTS:
- Clinical Case
- Overview of Taking a Sexual History
- Defining and Centering Sexual Health
- The Context of Taking A Sexual History in Clinical Settings
- Words Matter: Avoiding Judgmental and Stigmatizing Language
- Standardized Approaches to Sexual History-Taking
- The Wrap-Up
- Learn More – Primary Sources
- Glossary of Sexual History Terms and Language
THE CASE:
A 34-year-old cis-woman comes to your office for a routine check-up and STI screening. She is asymptomatic and denies any genitourinary symptoms or concerns.
- She married at a younger age and is now divorced. She has two young children and is taking her first steps towards returning to the dating world and sexual activity. She wants to discuss options where she can enjoy sex again but can also empower herself with tailored approaches to STI and HIV prevention
- She has always been attracted to both men and women, but only had sex with her husband for the 10 years they were married. She is open to either gender for a sexual relationship moving forward
- She has no medical conditions and is currently not taking any medications. She would consider condoms and birth control for contraception, but is interested in what may work best for her
Overview of Taking a Sexual History
The sexual history is a vital, yet often overlooked aspect of the clinical history and physical in medical settings
- Topics regarding sexuality, sexual orientation and behavior, and gender identity are vital aspects of the social history that can direct providers to identify
- sexual health and wellness recommendations
- screening tests
- tailored HIV and STI prevention approaches
- When it comes to HIV pre-exposure prophylaxis, or “PrEP,” it is impossible to hold a fluent conversation about HIV prevention before first becoming proficient in talking about sex
Defining and Centering Sexual Health
The definition of sexual health has been debated and modified over the years, but most sexual health experts refer to the World Health Organization (WHO) definition:
“Sexual health is fundamental to the overall health and well-being of individuals, couples and families, and to the social and economic development of communities and countries. Sexual health, when viewed affirmatively, requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence.”
- In many health professional schools, students have historically been taught to address sex from a pathological framework centered on disease states (i.e., HIV and STIs), screening for these conditions, and treating them appropriately
- Today’s approach to STI and HIV prevention and treatment now is proactive, focusing instead on sexual health, wellness, and prevention by creating spaces where patients feel more comfortable discussing their full and authentic selves
- Most people receiving new HIV diagnoses report contracting it through sexual transmission | To reduce the continued burden of STI and HIV rates, eliciting a good sexual history is crucial
The Context of Taking A Sexual History in Clinical Settings
When beginning as sexual history, it is important to recognize the complex dynamics that take place within the patient-clinician encounter:
- Patients prefer active inquiry about sexual health issues from clinicians (Ryan et al., 2018)
- Generational differences matter in communication about sexual health (Rabathaly and Chattu, 2019)
- Providers’ perception of how sexual history questions will be received by patients influences if a sexual history will be elicited and perceived competence led to more frequent screening (Tong et al., 2013)
- Sexual history-taking education in medical school curricula shows promise in improving students’ confidence in and comfort with conducting sexual histories with their patients (Bourne et al., 2020)
Competing interests and within-clinic demands also contribute to difficulty with competency in sexual history taking on a visit-by-visit basis:
- Not having enough time to discuss sensitive sexual information in a 15-minute clinical visit
- Building trust quickly without offending with personal questions
- Competing clinical priorities – chief complaint, other medical issues, health care maintenance
- Requirements for screening
- Interruptions from other clinical staff and other patients needing assistance
These contexts can put barriers in the way of clinicians having meaningful conversations with our patients around sexual health
- Learning to address these hurdles and incorporate language and behaviors in your practice will become easier with practice
- Implementation will, over the long term, will become seamless and improve the efficiency with which you take a sexual history
Routine review of sexual history can lead to improved patient outcomes
Words Matter: Avoiding Judgmental and Stigmatizing Language
Introductions
A provider’s approach to taking a comprehensive sexual history begins as soon as you introduce yourself to your patient
- Consider how we greet patients and the ways in which our perceptions of their physical appearance and gender expression leads to the insertion of the titles “Mr.” or “Mrs./Ms.” before their last name.
- Most of the time we guess correctly, but at times we may guess incorrectly and create a stigmatizing atmosphere for our patients before the full encounter even starts
- As a result, patients may shut down and not give a fully open and honest history; some may even question if they want to follow up with us altogether
We suggest an introduction like this: “Hi, my name is Dr./NP/PA _________________. My pronouns are she/her. What would you prefer to be called and what are your pronouns?”
- Using more open-ended language lets your patients know you are not assuming anything when it comes to their sexual and gender identities
- Additionally, it lets them know you respect them and will address them how they would like to be addressed, not based on your assumptions
When in doubt, ask patients how they prefer to be addressed | Never make assumptions.
Language
Language is key in sexual history-taking, and questions should be framed in open-ended and affirming language that allows patients to tell their own narrative:
- “I’m going to ask some personal questions about your sexual history now”
- “I ask these questions to all my patients to help get a sense of their sexual health needs”
- “What are the genders of your sexual partners”
- “What behaviors do you enjoy when having sex”
- “What forms of STI and HIV prevention do you use with your partners”
- “Do you have any specific sexual health concerns you want to talk about?”
Leading with open-ended questions avoids assuming certain sexual and gender identities (or the genders of their sexual partners):
- It allows patients to understand you are receptive to any response
- It creates a space where they will not be judged if they acknowledge having multiple sexual partners and regardless of the consistency of their HIV/STI prevention choices
- It allows communication to remain honest
- It facilitates identification of necessary testing, vaccination needs, and how to move forward with a sexual health and wellness plan that works for them
Standardized Approaches to Sexual History-Taking
There are many good resources to standardize the approach to sexual history-taking
The 5 P’s (CDC)
The most popular standardized approach to sexual history-taking comes from the CDC and is entitled “The 5 Ps” – which stand for:
- Partners
- Practices, including previous or current sex work
- Protection from STIs
- Past history of STIs
- Prevention of Pregnancy
These are commonly accepted categorization of the broad topics clinicians should cover during the encounter
- They are guidelines more than hard and fast rules, ensuring thorough content in a way that feels natural to the provider
- Flexibility is key to improve comfort and competence, including order of questions and wording
Essential Questions – Physicians for Reproductive Health
Physicians for Reproductive Health (PRH) suggests a template for sexual history-taking, particularly adolescents and emerging adults. They emphasize how to best set the atmosphere to ask sensitive sexual health questions, highlighting effective communication techniques that will help patients feel comfortable. These include:
- Minimize note-taking, particularly during sensitive questioning
- Talk in terms the adolescent will understand
- Ask developmentally appropriate questions
- Ask open-ended questions
- Practice listening skills
- Avoid the surrogate parent and adolescent roles
- It’s a conversation…not an interrogation!
- What purpose does the information serve?
- Healthy respect and regard for privileged information
Their recommended sexual history questions cover:
- Gender identity : “What names and pronouns do you use for yourself?”
- Sexual orientation “What genders are you interested in romantically?” and “Are you comfortable with your feelings?”
- Sexual coercion, abuse, and prior or current sex work “Who makes the decisions about when to have sex and what contraception to use?” and “have you exchanged sex for goods or services?” or “have you engaged in sex work in the past or currently?”
- Sexual activity
- Number of partners
- Frequency of intercourse
- Type of sex practices
- STI history and risk assessment “Have you ever been diagnosed with an infection?”
- Pregnancy history and risk assessment “Have you ever been pregnant or gotten anyone pregnant?” and “What are you doing to prevent pregnancy right now?”
- Contraceptive behaviors “What are your experiences with contraception to prevent pregnancy?”
- Substance use
Approaching the sexual history with respect, no assumptions, and a collaborative spirit will go a long way in fostering the trust needed for honest communication about sexual health and wellness
Note: It may be helpful to explain or collaborate with the patient on how the information they provide on their sexual health will be documented in the medical record to build trust
The Wrap-Up
The above patient will benefit from an open-ended sexual history
She is at a transitional time of her life where she is entering a new phase and would benefit from an affirming and empowering approach to her sexual health
- Start with a discussion of her current sexual and gender identities
- Explore what her sexual and romantic needs and desires are at this point
- Inquire regarding her concerns and worries about returning to dating and sexual activity after recently ending years of marriage
- Discuss her preferred approaches to contraception
- Evaluate her thoughts and preferred options for HIV and STI prevention (including PrEP) moving forward
KEY POINTS:
- STI and HIV prevention discussions begin with a sexual health conversation
- Patient-centered and tailored approaches should meet patients where they are
- Utilize affirming language over a judgmental and discriminatory tone
- Incorporate models of sexual history-taking that work best for your patients
Learn More – Primary Sources:
Centers for Diseases Control and Prevention
American College of Obstetricians and Gynecologists
Physicians for Reproductive Health
Human Rights Campaign Glossary of Terms
American Academy of Family Physicians
National LGBT Health Education Center
Glossary of Sexual History Terms and Language
When taking a sexual history, it is important to lead without assuming that everyone is cis-gendered and heterosexual. Approaching the questions and how to phrase them is the art of medicine, beginning with familiarizing oneself with key sexual orientation and gender identity (SOGI) terms that will help facilitate an open atmosphere in which patients feel comfortable discussing their sexual lives
Below is an abbreviated list of terms. A more expansive glossary is found on the HRC website. While it is possible that the majority of patients you encounter in clinical practice may identify as cis-gendered and heterosexual, it is paramount to create clinical spaces that are affirming and inclusive of all patients along the sexual and gender identity continuum. You may not need to use these terms with every patient and during your clinical sessions, but it is important to at least familiarize yourself with the terminology. This way we can service anyone’s sexual health needs and priorities, regardless of how they identify
According to the Human Rights Campaign (HRC), these are some basic terms and definitions around sexual identity and gender identity (SOGI) with which clinicians can familiarize themselves:
Sexual orientation | An inherent or immutable enduring emotional, romantic, or sexual attraction to other people
Lesbian | A woman who is emotionally, romantically, or sexually attracted to other women
Gay | A person who is emotionally, romantically, or sexually attracted to members of the same gender
Bisexual | A person emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity though not necessarily simultaneously, in the same way or to the same degree
LGBTQ | An acronym for “lesbian, gay, bisexual, transgender and queer”
Queer | A term people often use to express fluid identities and orientations. Often used interchangeably with “LGBTQ”
Gender identity | One’s innermost concept of self as male, female, a blend of both or neither—how individuals perceive themselves and what they call themselves. One’s gender identity can be the same or different from their sex assigned at birth
Cisgender | A term used to describe a person whose gender identity aligns with those typically associated with the sex assigned to them at birth
Transgender | An umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. Being transgender does not imply any specific sexual orientation. Therefore, transgender people may identify as straight, gay, lesbian, bisexual, etc.
Gender dysphoria | Clinically significant distress caused when a person’s assigned birth gender is not the same as the one with which they identify. According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), the term—which replaces Gender Identity Disorder—”is intended to better characterize the experiences of affected children, adolescents, and adults”
Gender expression | External appearance of one’s gender identity, usually expressed through behavior, clothing, haircut or voice, and which may or may not conform to socially defined behaviors and characteristics typically associated with being either masculine or feminine
Genderqueer | Genderqueer people typically reject notions of static categories of gender and embrace a fluidity of gender identity and often, though not always, sexual orientation. People who identify as “genderqueer” may see themselves as being both male and female, neither male nor female, or as falling completely outside these categories
Gender transition | The process by which some people strive to more closely align their internal knowledge of gender with its outward appearance. Some people socially transition, whereby they might begin dressing, using names and pronouns, and/or be socially recognized as another gender. Others undergo physical transitions in which they modify their bodies through medical interventions
Non-binary | An adjective describing a person who does not identify exclusively as a man or a woman. Non-binary people may identify as being both a man and a woman, somewhere in between, or as falling completely outside these categories. While many also identify as transgender, not all non-binary people do
Sex assigned at birth | The sex (male or female) given to a child at birth, most often based on the child’s external anatomy. This is also referred to as “assigned sex at birth”
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose
Special Thanks
Special thanks to David Malebranche, MD, MPH and Ariel Watriss, MSN, NP for their insights and contribution.

HIV Pre-Exposure Prophylaxis (PrEP) – Who’s it for?
Review the latest recommendations with
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
SUMMARY:
There are now three types of PrEP approved by the Food and Drug Administration (FDA) currently available – oral formulations (Truvada and Descovy) and an intramuscular injection, cabotegravir. All treatments work by stopping the HIV replication process. While HIV PrEP is recommended for all individuals that it is applicable for, at this time, Descovy is not approved for the prevention of HIV for those at risk through receptive vaginal sex – including cisgender women, transgender men, and others.
- Truvada brand name (Emtricitabine (F) 200mg with tenofovir disoproxil fumarate (TDF) 300mg) daily
- Descovy brand name (Emtricitabine (F) 200mg with tenofovir alafenamide (TAF) 25mg) daily
- Vocabria brand name (Cabotegravir 600mg) gluteal IM injection at month zero, month one, then every two months
Of note, we refer to Truvada as F/TDF, Descovy as F/TAF, and Vocabria as Cabotegravir throughout
BACKGROUND:
Providing Pre-exposure Prophylaxis
- Goal of PrEP is to reduce the acquisition of HIV and its subsequent costs to individuals and society
- PrEP has been a part of the HIV prevention landscape since 2012
- Both HIV PrEP oral tablets contain two antiretroviral medications called nucleoside reverse transcriptase inhibitors (NRTIs)
- These medications work by inhibiting the enzyme reverse transcriptase that HIV needs to replicate
- Both tablets are used in many common HIV treatment regimens
- The intramuscular injection contains an integrase strand-transfer inhibitor (INSTI) which works by inhibiting the enzyme that HIV uses to integrate its own DNA into the CD4 cell’s nucleic DNA
Oral PrEP medications
FDA Approved Regimens:
- Truvada | Emtricitabine (F) 200mg and tenofovir disoproxil (TDF) 300mg) | one tablet orally daily, with or without food
- Descovy | Emtricitabine (F) 200mg and tenofovir alafenamid (TAF) 25mg) | one tablet orally daily, with or without food
Alternative formulations of PrEP medications
Cabotegravir 600mg gluteal IM injection was granted FDA approval in December 2021
- Requires IM injection at month zero, month one, then every two months afterwards
- One three mL injection in the gluteal muscle
- Only available for HIV negative patients without contra-indications to the medication
What many clinicians wonder next is “What patients would be good candidates for PrEP?” PrEP is a sexual health option for people interested in HIV prevention and could be appropriate for many patients you see on a daily basis.
Who It’s For – CDC Guidance and Other Considerations
The CDC recently updated guidance to recommend routine counseling of risks of transmission of HIV and PrEP options as well as routine prescribing of PrEP to appropriate candidates. Now, discussion of PrEP is recommended for all individuals who are sexually active.
Although “risk groups” have been defined by the CDC, we caution the idea of patients as levels of “risk,” particularly when it comes to sexual health. What it involves is taking a good sexual history and documenting what behavioral choices they make, then offering PrEP as an option for HIV prevention.
PrEP is for people without HIV who could be exposed to HIV from sex or injection drug use.
The CDC provides the following recommendations:
CDC recommends the following patients should be assessed for PrEP including
- Sexually active gay and bisexual men without HIV
- Sexually active heterosexual men and women without HIV
- Sexually active transgender persons without HIV
- Persons without HIV who inject drugs
- Persons who have been prescribed non-occupational post-exposure prophylaxis (PEP) and report behaviors that could expose them to HIV, or who have used multiple courses of PEP
For sexually active adults and adolescents:
- Anal or vaginal sex in the past six months; and
- HIV-positive sexual partner (especially if partner has unknown or detectable viral load); or
- Recent bacterial STI; or
- History of inconsistent or no condom use with sexual partner(s)
For Persons who inject drugs:
- HIV-positive injecting partner; or
- Shares drug preparation or injection equipment
All persons eligible for PrEP:
- Documented negative HIV test result before prescribing PrEP; and
- No signs/symptoms of acute HIV infection; and
- Normal renal function; and
- No contraindicated medications
NOTE: While the CDC compartmentalizes “risk groups” as listed above, as clinicians we must remember that sexual health does not fit neatly into static compartments. Sexuality and sexual behavior are fluid, and individuals may change their partners, behavior, and condom use over time and situation – and invite us to explain in detail
Thus, the CDC guidance is exactly what it is – guidance. Nothing replaces taking a good sexual history to discover which patients may be good candidates for PrEP.
- Individuals who do not fit in the categories mentioned above could still benefit from PrEP – so be sure not to limit offering PrEP to just certain groups of people
- Anyone who is sexually active could be a candidate for PrEP.
- Patients who ask for PrEP may not feel comfortable sharing all their sexual behavior with medical providers due to fear of judgment and stigma
- If a patient comes into your office inquiring about PrEP, even if they don’t verbally describe specific behaviors that the CDC defines as “risky,” they are asking for a reason
Dosage Regimen
These medications are approved to prevent HIV infection in adults and adolescents weighing at least 35 kg (77 lb) as follows:
- Daily oral PrEP with F/TDF (Truvada) is recommended to prevent HIV infection among all persons at risk through sex or injection drug use.
- Daily oral PrEP with F/TAF (Descovy) is recommended to prevent HIV infection among persons at risk through sex, excluding people at risk through receptive vaginal sex. F/TAF has not yet been studied for HIV prevention for receptive vaginal sex.
Selecting a Regimen
- Determination of which oral regimen is appropriate depends on a patient’s clinical status, comorbidities, as well as potential side effects and medication interactions
- Both F/TDF and F/TAF are equally effective in reducing HIV transmission
- F/TDF (Truvada) is the only FDA-approved PrEP option for cis women who have receptive vaginal sex | May be better for people with a history of hypercholesterolemia
- F/TAF (Descovy) is FDA-approved for use by transgender women, transgender men, and MSM | the best option for persons with osteoporosis and can be used for patients with chronic kidney disease with a CrCl as low as 30 ml/min
- Comorbidities
- Hepatitis B
- HIV
- Renal disease
- Common side effects
- The majority of people experience no side effects at all
- Mild to moderate gastritis at start of med course- usually tapers within three to four weeks | Can sometimes include diarrhea
- Headaches
- Medication interactions
- Other drugs that could affect renal function may require closer renal function while PrEP is being used
- Other antiviral medications can impact PrEP response and need to be reviewed with clinical use on a case by case basis
“On-demand” PrEP
“On-demand” PrEP is not currently FDA-approved for use in the United States but many clinicians many use it in an “off-label” manner as appropriate with the needs of their patients and reflective of the studies in Europe that demonstrate its effectiveness in reducing HIV transmission.
- Would be an option for people who may not engage in sex regularly or plan sexual encounters
- Involves the following regimen schedule for TDF/FTC only
- Take two tablets at least two hours and not more than 24 hours before sex
- Take one tablet 24 hours after first two pills taken
- Take one tablet 48 hours after first two pills taken
PrEP Safety and Efficacy
PrEP, when used as indicated, has been determined to be safe and effective in the prevention of HIV transmission among diverse populations, including
- Men who have sex with men and transgender women: 85 – 100% risk reduction
- Heterosexual women and men: 63 – 90% risk reduction
- Persons who Inject Drugs (PWID) regardless of sexual activity: 73.5% risk reduction
- Adolescents who weigh over 35kg: >95% risk reduction
Clinical considerations with initiation
- Consider sexual health needs beyond HIV prevention- PrEP only offers prevention for HIV, not other STIs
- These medications must be monitored closely for patients with chronic active Hepatitis B (persistent positive Hepatitis B Surface Antigen)
- These medications require healthy kidney function (eCrCl >60 ml/min for TDF/FTC and eCrCl >30 ml/min for TAF/FTC)
- Can be prescribed by primary care providers without requiring infectious disease specialist or consult prior to initiation [for more information see Initial Visit, Dosing, and Follow Up or Implement and Maintain a Prep Clinic in the Resource Center]
- Cabotegravir, the intramuscular injection pending FDA approval, can be used in individuals without requiring creatinine or renal clearance, Hepatitis B status, lipid panels, or liver function tests
- Cabotegravir may be a better option for individuals who prefer injections every two months, have poor adherence with daily medication, or have other co-morbidities such as renal or liver disease
Learn More – Primary Sources:
CDC Pre-Exposure Prophylaxis for HIV Prevention
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose
Special Thanks
Special thanks to David Malebranche, MD, MPH and Ariel Watriss, MSN, NP for their insights and contribution.

Initial Visit, Dosing, and Follow Up
Review the latest recommendations with
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
SUMMARY:
The initial visit for HIV PrEP will establish the start of the patient’s PrEP experience. It is a blend of education, clinical care, and establishing a new health practice for the patient
Initial Visit: What to Include
The initial visit needs to include both a comprehensive history of the patient, their sexual history, eligibility for PrEP as well as laboratory workup prior to initiation
Sexual Health History and Comprehensive Screening
- A comprehensive sexual health history review and review of eligibility for PrEP includes
- Gender and number of sexual partners
- Specific sexual behaviors (oral, vaginal, anal)
- HIV-status of sexual partners
- Condom use practices
- Substance use/abuse screening
- History of sexually transmitted infections (STI)
- Confirmation of HIV negative status (see lab tests below)
- Assessment for acute HIV
- A patient’s HIV negative status must be confirmed in the context of recent sexual or other possible exposure contexts in the preceding thirty days
- If there is concern for acute HIV and someone has an initial negative HIV Ag/Ab, that may require HIV RNA testing before initiating PrEP
- Symptoms of acute HIV may include:
- Fever
- Pharyngitis
- Lymphadenopathy
- Many other symptoms (diarrhea, headache, flu-like symptoms) or NONE AT ALL
- Assessment for medical cautions or contraindications include
- Hepatitis B, renal or hepatic insufficiency
- Discussion with patients of potential, yet rare side effects, including:
- Truvada (F/TDF 200mg/300mg): worsening renal function including kidney failure, bone thinning
- Descovy (F/TAF 200mg/25mg): elevated cholesterol levels, weight gain
- Other sexual health needs including STI testing or contraception, as needed
Laboratory Tests and Other Diagnostic Procedures
Initiation of Oral PrEP
- HIV testing | must be performed and results must be negative within one week before starting PrEP to document that patients do not have HIV
- Fourth generation HIV Ag/Ab serologic testing is preferred over either oral/fingerstick rapid Ab or serologic Ab testing
- Renal function
- Truvada (F/FTC) | eCrCl should be documented at >60 ml/min prior to starting PrEP
- Descovy (F/TAF) | eCrCl should be >30 ml/min
- Hepatitis B surface antigen should be documented negative before initiating PrEP
- Both medications are active against Hepatitis B
- If an individual taking HIV PrEP also has chronic active Hepatitis B and suddenly stops PrEP, they could experience a symptomatic acute Hepatitis B flare
- Exhibit caution and educate patients about this dynamic if they have chronic active Hepatitis B
- Urine Pregnancy Test (UPT) for individuals who may become pregnant
- Sexually Transmitted Infection (STI) testing
- Hepatitis C antibody screening for PWID and MSM
Initiation of intramuscular PrEP
- Administration of cabotegravir 600mg via one 3mL intramuscular injection in the gluteal muscle
- Can consider trial of cabotegravir 30mg daily for four weeks prior to initiation of IM injections if patients are anxious about side effects
- Initiation of cabotegravir requires a second dose four weeks after the first dose (one month follow up visit) and every eight weeks after with HIV testing at visits
- Schedule is initial administration (month 0), one month after initiation (month one), then every eight weeks afterwards (month three, five, seven, etc.)
- Follow-up visit one month after initial injection should include second dose and HIV Ag/Ab test and HIV-1 RNA assay with subsequent two-month intervals
- The following laboratory tests are NOT indicated before starting CAB injection or for monitoring patients during its use:
- Creatinine or eCrCl
- hepatitis B serology
- lipid panels
- liver function tests
Medication choices and dosing
- The two current choices for oral PrEP are F/TDF 200/300 (Truvada) and F/TAF 200/25 (Descovy)
- Only F/TDF (Truvada) is FDA-approved for cis women engaging in vaginal sex
- Both are FDA-approved for men who have sex with men and transgender women
- Both are fixed-dose, daily tablets that can be taken with or without food
- Prescriptions can be written either as thirty days with two refills or as a ninety-day course depending on insurance coverage allowance
- Cabotegravir is now FDA-approved, administered at month zero, month one, then every two months (eight weeks) afterwards starting from month three, five, seven, etc.
Ongoing monitoring
The current recommendations for ongoing care for oral PrEP include:
- In-person or telehealth follow up visit every three months
- Prescription refills every three months
- HIV test every three months (typically done as part of refill of prescription on the same timeline and can be administered as at-home testing)
- Renal and hepatic labs every six months
- UPT as indicated
- STI testing as directed by sexual health review done at each follow up visit.
- Assessment of sexual and general health needs
- Review of any new medications and medical updates
Similar recommendations apply to intramuscular PrEP, with timing intervals every two months but would not require renal or hepatic lab results at initiation or during follow-up
Learn More – Primary Sources
ACHA Guidelines: HIV Pre-Exposure Prophylaxis
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose
Special Thanks
Special thanks to David Malebranche, MD, MPH and Ariel Watriss, MSN, NP for their insights and contribution.

The PrEP Guidelines Center
Review the latest recommendations with
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
SUMMARY:
The Centers for Disease Control and Prevention (CDC) makes recommendations for the use of PrEP as biomedical HIV prevention. Based on a systematic review of the literature, these evidence-based guidelines offer a practical approach to identifying patients who would be appropriate candidates for PrEP, ordering relevant tests and laboratory procedures, and how to conduct initial and follow-up visits for patients. Given the evolving nature of PrEP research, these recommendations will be revised and updated for clinical practice on a regular basis. This section will also review other supportive guidelines and statements from ACOG and USPSTF
General Guidelines for PrEP
Safety and Efficacy
PrEP, when used as indicated, has been determined to be safe and effective in the prevention of HIV transmission among diverse populations and should be a consideration to anyone who is sexually active, including:
- Men who have sex with men and transgender women: 92% to 100% reduction in HIV transmission in clinical trials and real-world analysis
- Heterosexual women and men – 63% to 93% reduction in HIV transmission
- Persons who Inject Drugs (PWID) – 73.5% reduction in HIV transmission
- Adolescents who weigh over 35kg – over 95% reduction in HIV transmission
Eligibility
The United States Prevention Services Task Force (USPSTF) recommends offering PrEP with effective antiretroviral therapy to persons at high risk of HIV acquisition
- FDA approved oral formulation is one pill taken once a day or intramuscular injection is once very eight weeks
- Either F/TDF 200/300mg (Truvada) or F/TAF 200/25 (Descovy) are currently approved for oral use and cabotegravir is approved for intramuscular use
- Insurance must provide medication coverage for preventive services with Grade A recommendation
CDC Guidelines for Screening Eligibility
- The CDC recommends that providers should
Inform all sexually active adults and adolescents that PrEP can protect them from getting HIV
Note: We caution against seeing patients as levels of “risk,” particularly when it comes to sexual health | What it involves is taking a good sexual history and documenting what behavioral choices they make, then offering PrEP as an option for HIV prevention
- PrEP is for people without HIV who could be exposed to HIV from sex or injection drug use
- CDC recommends the following should be assessed for PrEP including
- Sexually active gay and bisexual men without HIV
- Sexually active heterosexual men and women without HIV
- Sexually active transgender persons without HIV
- Persons without HIV who inject drugs
- Persons who have been prescribed non-occupational post-exposure prophylaxis (PEP) and report behaviors that could expose them to HIV, or who have used multiple courses of PEP
- For sexually active adults and adolescents
- Anal or vaginal sex in the past six months and
- HIV-positive sexual partner (especially if partner has unknown or detectable viral load) or
- Recent bacterial STI or
- History of inconsistent or no condom use with sexual partner(s)
- For persons who inject drugs
- HIV-positive injecting partner or
- Shares drug preparation or injection equipment
- All persons eligible for PrEP
- Documented negative HIV test result before prescribing PrEP and
- No signs/symptoms of acute HIV infection and
- Normal renal function and
- No contraindicated medications
Note: While the CDC compartmentalizes “risk groups” as listed above, clinicians should remember that sexual health does not fit neatly into static compartments | Sexuality and sexual behavior are fluid, and individuals may change their partners, behavior, and condom use over time and situations
Other Considerations
Follow-up
- Patients taking PrEP can be followed closely by medical staff who are both clinical and non-clinical to assure proper usage and safety
- Current recommended follow-up every three months for oral PrEP or every two months for intramuscular PrEP
- Use of in-person and telemedicine visits
- Specific laboratory testing is indicated upon initial visit and subsequent follow-up
Women’s Health
The American College of Obstetricians and Gynecologists (ACOG) recommends providers working with women at risk of HIV transmission be aware and up to date on this preventative health tool and encourage strong adherence as key to its effectiveness
Future Directions
- Future delivery systems of PrEP are in various stages of clinical development and research and will likely become available as options in the future:
- Long acting injectables – now FDA approved!
- Implants
- Long-acting oral agents
- Patches
Learn More – Primary Sources:
National Clinician Consulting Center: PrEP: Pre-Exposure Prophylaxis
National Institute of Health (NIH): Pre-Exposure Prophylaxis (PrEP)
World Health Organization (WHO) compendium of PrEP publications
ACOG: Preexposure Prophylaxis for the Prevention of Human Immunodeficiency Virus
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose
Special Thanks
Special thanks to David Malebranche, MD, MPH and Ariel Watriss, MSN, NP for their insights and contribution.

Implement and Maintain a PrEP Program in Your Clinic
Review the latest recommendations with
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
SUMMARY:
Pre-exposure prophylaxis (PrEP) should be viewed as a sexual health program that our patients can utilize. It involves integration of targeting sexual history-taking, comprehensive behavioral evaluations, and a discussion of a patient’s approach to achieving sexual pleasure while also incorporating HIV prevention options tailored to their needs
KEY POINTS:
- PrEP is a highly effective prevention tool that can reduce HIV transmission among our patients
- PrEP is a service that can be folded into a clinical practice similar to other specialized services
- Successful PrEP delivery requires passion, planning, and utilization of innovative delivery systems
- PrEP is an HIV prevention option that can be used by anyone who is sexually active
PrEP is a program, not a pill
PrEP Regimens
- Currently there are two daily oral PrEP regimens that patients can access and an intramuscular regimen every eight weeks
- F/TDF 200mg/300mg orally daily (Truvada)
- F/TAF 200mg/25mg orally daily (Descovy)
- Cabotegravir 600mg IM every eight weeks after initiation phase of administration at week zero and week four
- Promotes overall sexual health
- Monitors and screens actively for sexual transmitted infections (STIs)
- Serves as a gateway to normalizing routine health care
- Will soon involve other delivery systems beyond pills and injections
PrEP as a collaborative effort
- Involvement with local community-based organizations to create programs
- Continued involvement with community to evaluate and improve services
- Provision of other social programs can help assist in healthcare access
Innovative models
PrEP has been FDA-approved as an HIV prevention option since 2012
Traditional Models
- Traditional models for PrEP evaluation and distribution were primarily clinic-based
- over time these models have evolved to include approaches that provide more ways in which patients can access this sexual health option
Telemedicine
- Telemedicine: While telehealth models for PrEP were being explored earlier, the onset of the COVID-19 pandemic accelerated the use of telemedicine for PrEP services
- As an option for in person visits
- As a bridge between in person visits
- Coupled with at home HIV and STI testing
- Used to access “PrEP mentors” who provide expert guidance
Pharmacy-Based
- Pharmacy-based: Given the demand to see more patients placed on primary care providers in outpatient clinics, there may not be enough time for them to conduct a thorough sexual history and PrEP evaluation. PrEP programs that are pharmacist-led have been shown to be effective, as pharmacists are uniquely poised to bring a level of expertise that many clinicians may not have:
- Experienced guidance on medications, side effects, and drug interactions
- Familiarity with navigating the red tape PrEP with varied insurance plans
- Familiarity with patient assistance programs for patients who are uninsured or underinsured
Multi-disciplinary and other models
- Multidisciplinary models
- Community-led and maintained
- Peer-navigators facilitate linkage to care and continued engagement
- Nurse-led programs
Ongoing monitoring
See our post on Initial Visit, Dosing, and Follow-up for initiation of PrEP
The current recommendations for ongoing care once oral PrEP has been initiated include:
- In-person or telehealth follow up visit every three months
- Prescription refills every three months
- HIV test every three months (typically done as part of refill of prescription on the same timeline and can be administered as at-home testing)
- Renal and hepatic labs every six months
- UPT as indicated
- STI testing as directed by sexual health review done at each follow up visit.
- Assessment of sexual and general health needs
- Review of any new medications and medical updates
The current recommendations for ongoing care once IM PrEP has been initiated include all the above at two-month intervals except renal and hepatic lab monitoring
Practical Tip
While there is no “how-to” manual about starting and maintaining a PrEP program, there are some things you should consider when establishing one at your workplace:
- Personnel
- Recruit staff who are passionate and interested in doing sexual health & PrEP work
- Some of the routine follow ups and other visits do not have to be conducted by a medical provider
- You can have medical assistants and peer navigators involved as much as they would like
- Timing
- consider either integrating PrEP visits as part of everyday sessions OR make special clinic days or sessions devoted to seeing patients interested in PrEP
- You can always start small and ramp up available hours of service if needed
- Pharmacy
- Get pharmacy staff involved from the beginning throughout the process if you have a pharmacy on site
- Skilled pharmacists can help to navigate patients through patient assistance programs and copay cards as well as insurance coverage for generic versus brand name PrEP
- If you don’t have a pharmacy on-site, identify a local pharmacy who handles HIV and PrEP often to make the process easier for patients
Note: Mail-order delivery is a must-have option for many patients
- Optimize Electronic Medical Records
- Create “smart sets” for PrEP visits, both initial and follow-up
- This can help providers walk patients through appropriate history, physical exam details, and appropriate lab orders
- Telehealth is an essential aspect of many PrEP programs that allows for quick “check-ins” and other follow-up
- Ensures that patients have enough refills for PrEP
- Can identify what testing is necessary if they cannot make a visit in person
- Marketing
- Make sure your clinic’s website, waiting area, and exam rooms include information about PrEP services you offer will help ease some of the stigma patients may feel about asking about PrEP themselves
Learn More – Primary Sources:
Funding Resources
- National Institute of Health (NIH)
- Ending the HIV Epidemic (EHE)
- National Alliance of State and Territorial AIDS Directors (NASTAD)
Primary Sources
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose
Special Thanks
Special thanks to David Malebranche, MD, MPH and Ariel Watriss, MSN, NP for their insights and contribution.

Downloadable Infographics
For Healthcare Professionals | For Your Patients
Feel free to download and use these infographics
For Healthcare Professionals
Infographics for Your Patients

Take Control of Your Sexual Health
This information was prepared for you by
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
SUMMARY:
Who you have sex with and what kind of sex you have are your choices. Some things, like who else your partner or partners have sex with, are out of your control but can affect you. The group of infections that can be passed through sex have been called many different names: venereal diseases or VDs, sexually transmitted diseases or STDs, and sexually transmitted infections or STIs. On this site, we will call them STDs.
How You Can Take Control of your Sexual Health
- It’s possible to have sex with someone and not know they have an STD or HIV, but there are tools available that can help you take control of your sexual health
- When you take PrEP, you take control of your risk for HIV
- You choose your health care team
- You choose your PrEP medicine
- By checking in with your healthcare professional, you can make sure that
- PrEP is a good option and safe for you
- You check, treat, and control your risk for other STDs
- Making the decision to take control of your sexual health is powerful | Your sexual health is just as important as other parts of your health
- Some additional things you can discuss with your healthcare professional include
- Eating healthier
- Exercising more
- If you smoke, talk to your health care team about quitting
- If you use alcohol or other drugs, talk to your health care team about getting help to cut down or quit
- If you have depression, anxiety, or other mental health issues, work with your healthcare team so you can get the help that you need
- Vaccines can prevent serious infections, and new vaccine information comes out every year | Make sure with your health care team that you get all the vaccines that are right for you
- Remember that heart disease is the #1 killer in the US | Keeping your heart healthy can add years to your life
- If you have high blood pressure, work with your health care team to get it under control
- If you have diabetes, work with your health care team to manage your sugar
- If you have high cholesterol, work with your health care team to bring it down
Remember, you are driving this train. Do everything that you can to make sure that the ride is smooth, the journey is enjoyable, and that you reach your destination safely and in good health
Learn More – Primary Sources
There are many good websites with information for people interested in learning more about PrEP. Here are some.
CDC: PrEP (Pre-exposure Prophylaxis)
New York State Department of Health
PleasePrEPMe (California State)
CDC: PrEP Is for Women (cdc.gov)
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose

Women’s Health (PrEP to Protect You and Your Baby)
This information was prepared for you by
Jonathan Shuter, MD, a Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Uriel Felsen, MD, an Associate Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine
Raffaele M. Bernardo, DO, an Assistant Professor of Medicine in the Division of Infectious Diseases at Montefiore Medical Center and the Albert Einstein College of Medicine.
SUMMARY:
If you are thinking about getting pregnant, are pregnant, or have a baby, you are probably thinking a lot about both your health and the health of the baby. If you are trying to get pregnant and your partner is living with HIV, it is VERY important that you speak to your health care team about ways to lower the chance of HIV transmission. The group of infections that can be passed through sex have been called many different names: venereal diseases or VDs, sexually transmitted diseases or STDs, and sexually transmitted infections or STIs. On this site, we will call them STDs. In addition to HIV, other STDs, like herpes and syphilis, can also be dangerous for the baby. It is important that you speak with your health care team about controlling your risk for STDs and treating any you may have before, during, and after your pregnancy
What is PrEP?
- PrEP stands for Pre-Exposure Prophylaxis
- “Pre-exposure” means having medicine in your system even before you have sex
- “Prophylaxis” means the medicine prevents you from getting HIV even if your partner has it
What’s Changed?
- Until 2012
- The only ways to avoid getting HIV from sex were
- To not have sex
- Never have sex with someone with HIV
- Use condoms properly every single time
- And still … way too many people still got HIV from sex
- The only ways to avoid getting HIV from sex were
- Today, there are more ways to reduce your risk of HIV
- Newer medications for people with HIV that really work
- If your partner has HIV, make sure your partner takes HIV meds and has an undetectable HIV viral load | “Undetectable” means that the HIV virus cannot be found in the person’s blood
- Someone who STAYS undetectable by taking meds the right way can’t give anyone else the virus through sex
- Take PrEP to protect yourself if you don’t have HIV
- Newer medications for people with HIV that really work
More on PrEP
- When PrEP medicine is taken correctly it provides safe and excellent protection against HIV
- IF YOU DON’T TAKE IT, IT CAN’T WORK
- In most states, you cannot get PrEP without a physician prescription | In certain states, pharmacists may provide PrEP to people without a doctor’s prescription
What You Need to Know About PrEP Medications During Pregnancy
TDF/FTC (pills)
- TDF/FTC is one pill that contains 2 medicines and is also known as
- Truvada
- Tenofovir disoproxil fumarate/emtricitabine
- Takes about a week to build up to protective levels in your system, except in the vagina where it can take three weeks
- TDF has been used as a medicine for HIV since 2001 and FTC since 2004
- These meds have been around for a long time
- Use of TDF/FTC in pregnancy
- Many pregnant women have used TDF/FTC, both women living with HIV and women on PrEP
- It is considered safe for both mom and baby
- Less is known about TDF/FTC if you’re breastfeeding (more below)
Cabotegravir (injection)
- Cabotegravir injection is also known as
- Apretude
- CAB-LA
- Has been used in the US as a medicine for HIV since January 2021
- Cabotegravir use in pregnancy
- Has been used by very few pregnant and breastfeeding women
- There is no sign yet of any significant risk, but it is too early to say anything about its safety with confidence
Note: TAF/FTC is another combination pill that is effective at preventing HIV but has not been approved as a PrEP medication for vaginal sex, so TDF/FTC and cabotegravir are the only medicines for use in people who are or are trying to get pregnant
If You are Already on PrEP Medication During the Time You are Trying to Get Pregnant
TDF/FTC
- Continue it unless you, together with your health care team, decide that the chance of HIV transmission from your partner(s) is extremely low, such as
- If you stop having sex during pregnancy
- If your partner is HIV negative (and both you and your partner have no other partners)
- If your partner is living with HIV, takes meds consistently and correctly, and has kept an undetectable viral load
Note: Remember that it will take up to three weeks to be safely back on PrEP again if you decide to restart it
Cabotegravir
- Discuss with your health care team whether to
- Continue
- Stop
- Switch to TDF/FTC
Breastfeeding
- TDF/FTC
- Appears to be safe for mom and baby if you are breastfeeding
- However, there is not enough experience to know for sure
- Cabotegravir
- Almost nothing is known about cabotegravir and breastfeeding since this is a newer medication
Note: If you are thinking about taking PrEP and breastfeeding, you should discuss this with your health care team, including your baby’s pediatrician
Learn More – Primary Sources
There are many good websites with information for people interested in learning more about PrEP. Here are some.
CDC: PrEP Is for Women (cdc.gov)
CDC: PrEP (Pre-exposure Prophylaxis)
International Association of Providers of AIDS Care (iapac.org): Pre-Exposure Prophylaxis (PrEP)
New York State Department of Health
PleasePrEPMe (California State)
Commercial Support
This educational activity is supported by an independent educational grant from Gilead Sciences
Faculty Disclosures
Dr. Shuter has no relevant financial relationships to disclose
Dr. Felsen has no relevant financial relationships to disclose
Dr. Bernardo has no relevant financial relationships to disclose